Administration of Nitrates After Spontaneous Delivery in Rheumatic Heart Disease
Downloads
Introduction: Heart disease is one of the most common causes of maternal death. The incidence has increased since women with congenital and acquired heart disease reached fertile age. The circulation system changes during pregnancy which are induced by changes in the progesterone. The changes in progesterone levels increase heart work and cause death in pregnant women. Objective: This report aims to elaborate on the administration of nitrates as the management of labor in rheumatic heart disease (RHD). Case Report: A 27-year-old woman complained of shortness of breath and wanted to give birth. The patient was 38 weeks pregnant and had a history of heart disease. Antero-posterior chest radiography examination showed pulmonary edema and cardiomegaly. The patient was examined using echocardiography before spontaneous labor and was diagnosed as pregnant with rheumatic heart disease. As an emergency management, the patient was given painless spontaneous labor. The patient was given nitrates on the first day after delivery as a treatment for progesterone withdrawal syndrome in this case. After the delivery process was completed, the patient was admitted to the Intensive Care Unit (ICU). Progesterone hormone produced by the corpus luteum and the placenta until the eighth week of pregnancy and before delivery, respectively, can reduce systemic vascular resistance. Progesterone hormone increase causes peripheral vasodilation by affecting the function of endothelial nitric oxide synthase (eNOS) and nitrite oxide (NO) production. Conclusion: A pregnant woman with rheumatic heart disease can be given exogenous nitrate. Administration of exogenous nitrates in this patient successfully prevent the reduction of peripheral vascular resistance and postpartum hemodynamic instability because it can replace the reduction in nitric oxide caused by progesterone withdrawal.
Khatun J. A 25-Year-Old Pregnant Lady with Heart Disease. Journal of Enam Medical College. 2017;7(1):42–3.
Huisman CM, Zwart JJ, Roos-Hesselink JW, Duvekot JJ, van Roosmalen J. Incidence and Predictors of Maternal Cardiovascular Mortality and Severe Morbidity in the Netherlands: A Prospective Cohort Study. PLoS One. 2013 Feb 14;8(2).
Hu H, Pasca I. Management of Complex Cardiac Issues in the Pregnant Patient. Vol. 32, Critical Care Clinics. W.B. Saunders; 2016. p. 97–107.
Kumar RK, Tandon R. Rheumatic fever & rheumatic heart disease: The last 50 years. Indian Journal of Medical Research. 2013;137(4):643–58.
Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, de Bonis M, et al. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Vol. 39, European Heart Journal. Oxford University Press; 2018. p. 3165–241.
Kodogo V, Azibani F, Sliwa K. Role of pregnancy hormones and hormonal interaction on the maternal cardiovascular system: a literature review. Clinical Research in Cardiology [Internet]. 2019;108(8):831–46. Available from: http://dx.doi.org/10.1007/s00392-019-01441-x.
Grattan DR, Ladyman SR. Neurophysiological and cognitive changes in pregnancy [Internet]. 1st ed. Vol. 171, Handbook of Clinical Neurology. Elsevier B.V.; 2020. 25–55 p. Available from: http://dx.doi.org/10.1016/B978-0-444-64239-4.00002-3.
Clarissa Dass, Arun Kanmanthareddy. Rheumatic Heart Disease. StatPearls; 2022.
Chen RS, Bivens MJ, Grossman SA. Diagnosis and management of valvular heart disease in emergency medicine. Emerg Med Clin North Am. 2011;29(4):801–10.
Gottlieb M, Long B, Koyfman A. Evaluation and Management of Aortic Stenosis for the Emergency Clinician: An Evidence-Based Review of the Literature. Journal of Emergency Medicine [Internet]. 2018;55(1):34–41. Available from: https://doi.org/10.1016/j.jemermed.2018.01.026.
Ashrafi R, Curtis SL. Heart Disease and Pregnancy. Cardiol Ther. 2017;6(2):157–73.
Lloyd JW, Nishimura RA, Borlaug BA, Eleid MF. Hemodynamic Response to Nitroprusside in Patients with Low-Gradient Severe Aortic Stenosis and Preserved Ejection Fraction. J Am Coll Cardiol [Internet]. 2017;70(11):1339–48. Available from: http://dx.doi.org/10.1016/j.jacc.2017.07.736.
Copyright (c) 2023 Mirza Koeshardiandi, Muhammad Wildan Afif Himawan, Fajar Perdhana, Zulfikar Loka Wicaksana

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
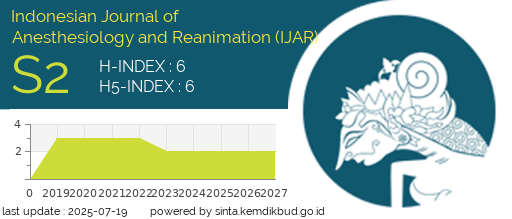
Indonesian Journal of Anesthesiology and Reanimation (IJAR) licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
1. Copyright holder is the author.
2. The journal allows the author to share (copy and redistribute) and adapt (remix, transform, and build) upon the works under license without restrictions.
3. The journal allows the author to retain publishing rights without restrictions.
4. The changed works must be available under the same, similar, or compatible license as the original.
5. The journal is not responsible for copyright violations against the requirement as mentioned above.