Perioperative Anesthetic Management in Repair Diaphragmatic Hernia with Atrial Septal Defect and Pulmonary Hypertension
Downloads
Introduction: Patients who had suffered disease of atrial septal defect (ASD) coming by pulmonary hypertension (PH) often present a clinical dilemma. Both of these disorders are congenital anomalies that often appear in pediatrics. Anaesthetic management in diaphragmatic hernia repair with this comorbidity requires precision and accuracy to avoid morbidity and mortality during surgery. The right management and care of anesthetic procedures is needed for patients who will be operated on with these two disorders. Objective: To describe the anesthetic management of a diaphragmatic hernia repair patient with comorbid ASD and pulmonary hypertension. Case report: The patient, a 1.5-month-old female baby born, has presented with shortness of breath complaints since the birth. Those were born spontaneously at the midwife's office and did not cry immediately, and a history of blueing and decreased consciousness was admitted for 20 days. Based on the examination, the diagnosis of diaphragmatic hernia from echocardiography found ASD and PH with a left ventricular ejection fraction of 64%. The patient was planned for diaphragmatic hernia repair under general anesthesia. Induction of anesthesia was performed with 5 mcg of fentanyl and inhalation anesthetic 3.5 vol% sevoflurane. After the endotracheal tube (ETT) was attached, the patient was desaturated to 50%, then the hyperventilated oxygenation was performed and positioned with knee chest position, and then milrinone at a dose of 1 mcg/min was given, saturation rose to 100%. During intraoperative ventilation control with manual bagging and maintenance anesthesia with inhalation ansethetic sevoflurane of 3.2 vol%. After surgery, the patient was admitted and observed in the pediatric intensive care unit for 2 days before extubation. Conclusion: Appropriate perioperative management in ASD patients with PH can reduce perioperative morbidity and mortality.
Kaoukabi A El, Menfaa M, Hasbi S, Sakit F, Choho A. Acute Gastric Volvulus on Hiatal Hernia. Case Rep Surg. 2020; 2020 (4141729): 1–5. [PubMed]
Fendy. Repair Defek Hernia Diafragmatika Dengan Kombinasi Anestesi Epidural Torakal Dan Intubasi Endotrakeal. UMI Med J. 2018;3(2):1–16. [WebPage]
Köckerling F, Simons MP. Current Concepts of Inguinal Hernia Repair. Visc Med. 2018; 34(2): 145–50. [PubMed]
Rajagopal S, Ruetzler K, Ghadimi K, Horn EM, Kelava M, Kudelko KT, et al. Evaluation and Management of Pulmonary Hypertension in Noncardiac Surgery: A Scientific Statement from the American Heart Association. Circulation. 2023; 147(17): 1317–43. [PubMed]
Ma Z, Viswanathan G, Sellig M, Jassal C, Choi I, Garikipati A, et al. β-Arrestin–Mediated Angiotensin II Type 1 Receptor Activation Promotes Pulmonary Vascular Remodeling in Pulmonary Hypertension. JACC Basic to Transl Sci. 2021; 6(11): 854–69. [PubMed] [WebPage]
Smilowitz NR, Armanious A, Bangalore S, Ramakrishna H, Berger JS. Cardiovascular Outcomes of Patients With Pulmonary Hypertension Undergoing Noncardiac Surgery. Am J Cardiol [Internet]. 2019; 123(9): 1532–7. [PubMed] [WebPage]
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, et al. 2022 ESC/ ERS Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension Developed by the Task Force for the Diagnosis and Treatment of (ESC) and the European Respiratory Society (ERS). Eur Heart J. 2022; 43(38): 3618–731. [PubMed] [WebPage]
Cartin-Ceba R, Krowka MJ. Portopulmonary hypertension. Clin Liver Dis [Internet]. 2014; 18(2): 421–38. [WebPage] [PubMed]
Gattinoni L, Collino F, Maiolo G, Rapetti F, Romitti F, Tonetti T, et al. Positive end-expiratory pressure: How to set it at the individual level. Ann Transl Med. 2017; 5(14). [PubMed]
Bandyopadhyay D, Lai C, Pulido JN, Restrepo-Jaramillo R, Tonelli AR, Humbert M. Perioperative approach to precapillary pulmonary hypertension in non-cardiac non-obstetric surgery. Eur Respir Rev [Internet]. 2021; 30(162). [WebPage] [PubMed]
Shah SB, Chowdhury I, Bhargava AK, Sabbharwal B. Comparison of hemodynamic effects of intravenous etomidate versus propofol during induction and intubation using entropy guided hypnosis levels. J Anaesthesiol Clin Pharmacol. 2015; 31(2): 180–5. [PubMed] [WebPage]
De Wit F, Van Vliet AL, De Wilde RB, Jansen JR, Vuyk J, Aarts LP, et al. The effect of propofol on haemodynamics: Cardiac output, venous return, mean systemic filling pressure, and vascular resistances. Br J Anaesth. 2016; 116(6): 784–9. [PubMed] [WebPage]
Jor O, Maca J, Koutna J, Gemrotova M, Vymazal T, Litschmannova M, et al. Hypotension after induction of general anesthesia: occurrence, risk factors, and therapy. A prospective multicentre observational study. J Anesth [Internet]. 2018;32(5):673–80. [WebPage] [PubMed]
Schulte-Sasse U, Hasse W, Tarnow J. Pulmonary Vascular Responses to Nitrous Oxide in Patients with Normal and High Pulmonary Vascular Resistance. Anesthesiology. 1982; 57(1): 9–13. [PubMed]
Inada T, Inada K, Kawachi S, Takubo K, Tai M, Yasugi H. Haemodynamic comparison of sevoflurane and isoflurane anaesthesia in surgical patients. Can J Anaesth. 1997; 44(2): 140–5. [PubMed]
Malan PT, DiNardo JA, Isner JR, Frink EJ, Goldberg M, Fenster PE, et al. Cardiovascular Effects of Sevoflurane Compared with Those of Isoflurane in Volunteers. Anesthesiology. 1995; 83(5): 918–28. [PubMed] [WebPage]
Petit PC, Fine DH, Vásquez GB, Gamero L, Slaughter MS, Dasse KA. The Pathophysiology of Nitrogen Dioxide during Inhaled Nitric Oxide Therapy. ASAIO J. 2017; 63(1): 7–13. [PubMed]
Buckley MS, Agarwal SK, Garcia-Orr R, Saggar R, MacLaren R. Comparison of Fixed-Dose Inhaled Epoprostenol and Inhaled Nitric Oxide for Acute Respiratory Distress Syndrome in Critically Ill Adults. J Intensive Care Med. 2021; 36(4): 466–76. [PubMed] [WebPage]
Thunberg C, Morozowich S, Ramakrishna H. Inhaled therapy for the management of perioperative pulmonary hypertension. Ann Card Anaesth. 2015; 18(3): 394–402. [PubMed] [WebPage]
Sarkar MS, Desai PM. Pulmonary hypertension and cardiac anesthesia: Anesthesiologist’s perspective. Ann Card Anaesth. 2018; 21(2): 116–22. [PubMed]
Sugawara Y, Mizuno Y, Oku S, Goto T. Effects of vasopressin during a pulmonary hypertensive crisis induced by acute hypoxia in a rat model of pulmonary hypertension. Br J Anaesth. 2019; 122(4): 437–47. [PubMed] [WebPage]
Rieg AD, Suleiman S, Perez-Bouza A, Braunschweig T, Spillner JW, Schrod̈er T, et al. Milrinone relaxes pulmonary veins in guinea pigs and humans. PLoS One. 2014; 9(1): 1–11. [PubMed] [WebPage]
Miller-Hance W. Anesthesia for Noncardiac Surgery in Children With Congenital Heart Disease. A Pract Anesth Infants Child. 2018; 534: 559.e9. [WebPage]
Brown ML, DiNardo JA, Nasr VG. Anesthesia in Pediatric Patients With Congenital Heart Disease Undergoing Noncardiac Surgery: Defining the Risk. J Cardiothorac Vasc Anesth [Internet]. 2020; 34(2): 470–8. [WebPage]
Copyright (c) 2024 M Irvan Noorrahman, Pratama Ananda, Novita Anggraeni

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
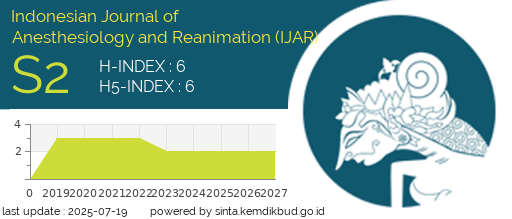
Indonesian Journal of Anesthesiology and Reanimation (IJAR) licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
1. Copyright holder is the author.
2. The journal allows the author to share (copy and redistribute) and adapt (remix, transform, and build) upon the works under license without restrictions.
3. The journal allows the author to retain publishing rights without restrictions.
4. The changed works must be available under the same, similar, or compatible license as the original.
5. The journal is not responsible for copyright violations against the requirement as mentioned above.