HEALTH FINANCING ANALYSIS OF MINIMUM SERVICE STANDARDS IN THE HEALTH SECTOR
Background: This research focuses on health financing Minimum Service Standards (MSS) in the health sector in Lumajang Regency, Indonesia, spanning 2019 to 2022. Despite the government's emphasis on Health MSS, disparities in service access and health conditions persist across different regions.
Aims: The research aims to provide insights into the effectiveness of health financing, serving as a foundation for policy recommendations to enhance the efficiency and effectiveness of health fund allocation in Lumajang Regency.
Methods: The research employs a quantitative descriptive approach, utilizing DHA and CBA. The study also investigates the budget allocation for MSS Health services.
Results: The findings of the research reveal that the realization of Local Original Revenue (LOR) in the Health sector tends to fall below targets. Non-Physical DAK dominate the funding sources in Community Health Centers (Puskesmas). Maternal health services receive the highest MSS Health budget allocation, but the spending proportion relative to total health expenditure is decreasing.
Conclusion: The research underscores the importance of addressing disparities in health financing and service access in Lumajang Regency. Recommendations include the diversification of funding sources, optimization of financing at the Puskesmas level, and a reevaluation of the budget allocation for maternal health services.
Keywords: CBA, DHA, health financing analysis, minimum service standards
Introduction
Quality health services are a fundamental prerequisite for achieving societal well-being. In this context, the health sector’s Minimal Service Standards (MSS) are a crucial benchmark(Organization, 2022). MSS in Health, as regulated by Minister of Health Regulation No. 4 of 2019, mandates that every citizen is entitled to basic health services of a minimal type and quality. However, despite Health MSS being a government priority to narrow regional gaps, on-the-ground realities still reveal significant disparities in service access and health conditions across various regions. The implementation of MSS poses a complex challenge, particularly concerning local health financing schemes(Myloneros & Sakellariou, 2021). In this context, the study of local health financing schemes in Indonesia becomes a focal point of interesting debate. Local governments are responsible for planning, financing, and distributing health services, but policy complexity and local political interests influence their role in health financing allocation Sunarto, 2020(Santinha & , 2023). In an effort to achieve Health MSS targets, the central government's role in health financing regulation remains dominant. In Lumajang Regency, despite an increase in the regional budget value in recent years, the budget allocation for health MSS has not seen a proportional increase.
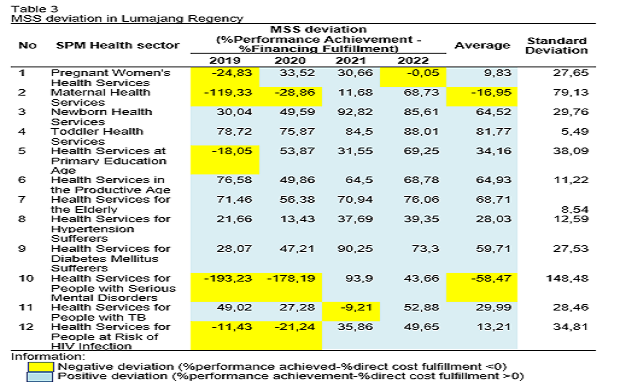
The data show that health financing in Lumajang Regency is still far from the desired target, as reflected in the decreasing percentage of the budget allocated to health MSS from year to year. Reconciliation results of the Regional Budget Implementation of Lumajang Regency (2019-2022) reveal data for Health MSS financing recorded as 5.89% of the regional government's health budget in 2019 (amounting to IDR 19,871,181,718 out of a total of IDR 337,220,278,143.91). Subsequently, in 2020, it was 3.94% of the regional government's health budget (amounting to IDR 13,175,653,782 out of a total of IDR 334,306,388,483.6). In 2021, it was only 2.01% of the regional government's health budget (amounting to IDR 8,525,902,328 out of IDR 423,663,017,207.13). The latest data for 2022 show a further decrease to 1.89% of the regional government's health budget (amounting to IDR 7,963,801,042 out of IDR 421,720,186,525.47)(Lumajang, 2022).
Reconciliation results of budget and Health MSS realization data from 2019 to 2022 indicate significant fluctuations, with some Health MSS indicators still below 50% of the target. This condition raises serious concerns, especially when compared to the monitoring and evaluation results of the Lumajang Regency Health MSS team, noting that the performance of the Health MSS program has not yet reached the 100% target. Therefore, this study delves deeper into the health financing scheme in Lumajang Regency. The primary focus will be on District Health Account (DHA) analysis as a tool to understand health fund flows systematically(Haryani et al., 2022)(Gani, 2022). Additionally, the Cost and Benefit Analysis (CBA) approach will be applied to measure the economic efficiency of basic health services and evaluate the impact of investments in fulfilling Health MSS financing(Brent, 2023). This study is expected to reveal a clearer connection between health financing schemes, the fulfillment of Health MSS targets, and the economic impact of these investments(Darrudi et al., 2022). Better alignment between programs, activities, outputs, and outcomes is anticipated through comprehensive and evidence-based analysis(Lundmark & , 2021). This serves as an important initial step to enhance the effectiveness and efficiency of resource utilization in achieving Health MSS targets in Lumajang Regency(Xu & , 2018).
Method
This research employed a descriptive research design with a quantitative analysis approach to provide an overview or description of government-sourced health financing in the implementation of Minimal Service Standards (MSS) in the health sector in Lumajang Regency from 2019 to 2022. The integrated approach includes a District Health Account (DHA) and Cost- Benefit Analysis (CBA) with a focus on income allocation, expenditure allocation, and budget expenditure appropriateness(Murniati et al., 2020). Secondary data used are derived from MSS Health budget documents in Lumajang Regency from 2019 to 2022. Secondary data collection involves instruments in the form of data collection forms prepared by the researchers. Data analysis was carried out through pivot tables, considering nine dimensions of the District Health Account (DHA), involving funding sources, budget managers, service providers, types of activities, budget items, programs, activity levels, and beneficiaries(John & , 2019).
The research was conducted in the Lumajang Regency Government, involving the Health Office and Community Health Centers. The research period extended from January to September 2023, covering the permission process, primary data collection, data cleaning and processing, data analysis, and result writing. The research object is MSS Health service activities in the Health Office and Community Health Centers in Lumajang Regency. Data processing used a computer with simple calculations using pivot tables, followed by data analysis(Palupi & , 2020). Identification of costs and benefits was conducted to illustrate the comparison between total costs and total benefits received from MSS Health financing(Hauck & , 2019).
After identifying the value of benefits and costs, a Benefit-Cost Ratio (BCR) calculation was performed to evaluate whether the benefits are proportional to the investment made(Rahmiyati & , 2018). BCR was calculated by comparing total benefits with total costs. Research ethics approval involves informed consent, anonymity, and confidentiality of research subject information. This research has been submitted to the Ethics Commission of the Faculty of Dentistry, University of Jember. The analysis was conducted to assess the cost requirements for meeting the targets of the
AbdulRaheem, Y. (2023) ‘Unveiling the Significance and Challenges of Integrating Prevention Levels in Healthcare Practice', Journal of Primary Care & Community Health, 14, p. 21501319231186500. Available at: https://doi.org/10.1177/21501319231186500.
Amin, H.I.M. and Cek, K. (2023) ‘The Effect of Golden Ratio-Based Capital Structure on Firm's Financial Performance', Sustainability (Switzerland), 15(9). Available at: https://doi.org/10.3390/su15097424.
Au Yong, H.N. et al. (2021) ‘The Impact of Socioeconomic Factors on Public Health Care Expenditure in Asean Countries', Journal of Environmental Science and Sustainable Development, 4(2), pp. 195–221. Available at: https://doi.org/10.7454/jessd.v4i2.1104.
Brent, R.J. (2023) ‘Cost-Benefit Analysis versus Cost-Effectiveness Analysis from a Societal Perspective in Healthcare', International Journal of Environmental Research and Public Health, 20(5). Available at: https://doi.org/10.3390/ijerph20054637.
Clark, R., Reed, J. and Sunderland, T. (2018) ‘Bridging funding gaps for climate and sustainable development: Pitfalls, progress and potential of private finance', Land Use Policy, 71, pp. 335–346. Available at: https://doi.org/10.1016/j.landusepol.2017.12.013.
Cristea, M. et al. (2020) ‘The Impact of Population Aging and Public Health Support on EU Labor Markets', International Journal of Environmental Research and Public Health, 17(4), p. 1439. Available at: https://doi.org/10.3390/ijerph17041439.
Darrudi, A., Ketabchi Khoonsari, M.H. and Tajvar, M. (2022) ‘Challenges to Achieving Universal Health Coverage Throughout the World: A Systematic Review', Journal of Preventive Medicine and Public Health, 55(2), pp. 125–133. Available at: https://doi.org/10.3961/jpmph.21.542
Gani, A. (2022) Pedoman DHA (District Health Account). Jakarta: UI Press.
Gooding, K. et al. (2022) ‘How can we strengthen partnership and coordination for health system emergency preparedness and response? Findings from a synthesis of experience across countries facing shocks', BMC Health Services Research, 22(1). Available at: https://doi.org/10.1186/s12913-022-08859-6.
Haryani, N., Nasution, S.W. and Ginting, C.N. (2022) ‘Analysis of Government Sourcing Health Financing With District Health Account (DHA) Approach in Deli Serdang Regency, 2018-2020', International Journal of Health and Pharmaceutical (IJHP), 2(4), pp. 718–722. Available at: https://ijhp.net/index.php/IJHP/article/view/90.
Hauck, K. et al. (2019) ‘How can we evaluate the cost-effectiveness of health system strengthening? A typology and illustrations', Social Science and Medicine, 220, pp. 141–149. Available at: https://doi.org/10.1016/j.socscimed.2018.10.030.
Hyeda, A., Da Costa, í‰.S.M. and Kowalski, S.C. (2022) ‘The trend and direct costs of screening and chemotherapy treatment of breast cancer in the new coronavirus pandemic: total and interrupted time series study', BMC Health Services Research, 22(1), p. 1466. Available at: https://doi.org/10.1186/s12913-022-08884-5.
Indriyanti, D. (2023) ‘Management of Non-Physical Special Allocation Funds for the Health Sector Health Operational Assistance at Community Health Centers during the Pandemic Period', International Journal of Integrative Sciences, 2(3), pp. 325–338. Available at: https://doi.org/10.55927/ijis.v1i4.3587.
John, S.K. et al. (2019) Feasibility Study for the Consolidation of Military Medical Education and Training Organizations, Functions, and Activities (Revised). Institute for Defense Analyses, pp. i–ii. Available at: https://www.jstor.org/stable/resrep22861.1.
Kruk, M.E. et al. (2018) ‘High-quality health systems in the Sustainable Development Goals era: time for a revolution', The Lancet Global Health, 6(11), pp. e1196–e1252. Available at: https://doi.org/10.1016/S2214-109X(18)30386-3.
Légaré, F. et al. (2018) ‘Interventions for increasing the use of shared decision making by healthcare professionals', The Cochrane database of systematic reviews, 7, p. CD006732. Available at: https://doi.org/10.1002/14651858.CD006732.pub4.
Lundmark, R. et al. (2021) ‘Alignment in implementation of evidence-based interventions: a scoping review', Implementation Science, 16(1), p. 93. Available at: https://doi.org/10.1186/s13012-021-01160-w.
Murniati, N.N., Indrayathi, P.A. and Januraga, P.P. (2020) ‘Analysis of Public Health Centre Financing using the District Health Account (DHA) Model in Karangasem District, Bali, Indonesia', Public Health and Preventive Medicine Archive, 8(1), pp. 66–71. Available at: https://doi.org/10.15562/phpma.v8i1.256.
Myloneros, T. and Sakellariou, D. (2021) ‘The effectiveness of primary health care reforms in Greece towards achieving universal health coverage: a scoping review', BMC Health Services Research, 21(1). Available at: https://doi.org/10.1186/s12913-021-06678-9.
Palupi, J. et al. (2020) ‘The effectiveness of literacy stimulation model based on multisensory development of the results of DDST', in Journal of Physics: Conference Series. Institute of Physics Publishing. Available at: https://doi.org/10.1088/1742-6596/1563/1/012056.
Pemkab Lumajang (2022) Laporan Realisasi Anggaran Pendapatan dan Belanja Daerah. Lumajang: Pemkab Lumajang.
Rahmiyati, A.L. et al. (2018) ‘Cost Benefit Analysis (CBA) Program Pemberian Makanan Tambahan (PMT) Susu Pada Karyawan di PT. Trisula Textile Industries Tbk Cimahi Tahun 2018', Jurnal Ekonomi Kesehatan Indonesia, 3(1).
Santinha, G. et al. (2023) ‘Designing a Health Strategy at Local Level: A Conceptual Framework for Local Governments', International Journal of Environmental Research and Public Health, 20(13), p. 6250. Available at: https://doi.org/10.3390/ijerph20136250.
Syafrawati, S. et al. (2023) ‘Factors driving and inhibiting stunting reduction acceleration programs at district level: A qualitative study in West Sumatra', PLoS ONE, 18(3 MARCH). Available at: https://doi.org/10.1371/journal.pone.0283739.
Tandon, A. and Reddy, K.S. (2021) ‘Redistribution and the health financing transition', Journal of global health, 11, p. 16002. Available at: https://doi.org/10.7189/jogh.11.16001.
World Health Organization (2022) Indonesia TB Joint External Monitoring Mission (JEMM) Report. WHO Indonesia. Available at: https://www.who.int/indonesia/news/publications/other-documents/tb-joint-external-monitoring-mission-(jemm)-report--2022.
Xu, X. et al. (2018) ‘Evaluation of health resource utilization efficiency in community health centers of Jiangsu Province, China', Human Resources for Health, 16(1). Available at: https://doi.org/10.1186/s12960-018-0275-y.
Yaghoubi, M. et al. (2023) ‘Providing a model for financing the treatment costs during biological crises using the fiscal space development approach', Health Economics Review, 13(1). Available at: https://doi.org/10.1186/s13561-023-00450-x.
Zawudie, A.B. et al. (2022) ‘Economic Burden of Diabetic Mellitus Among Patients on Follow-up Care in Hospitals of Southwest Shewa Zone, Central Ethiopia', BMC Health Services Research, 22(1), p. 1398. Available at: https://doi.org/10.1186/s12913-022-08819-0.
Zeng, W. et al. (2020) ‘Improving Fiscal Space for Health from The Perspective of Efficiency in Low- and Middle-Income Countries: What is The Evidence?', Journal of Global Health, 10(2), pp. 1–10. Available at: https://doi.org/10.7189/jogh.10.020421.
Copyright (c) 2024 Arie Risdiyanti, Hadi Paramu, Sunarto Sunarto

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
1. As an author you (or your employer or institution) may do the following:
- make copies (print or electronic) of the article for your own personal use, including for your own classroom teaching use;
- make copies and distribute such copies (including through e-mail) of the article to research colleagues, for the personal use by such colleagues (but not commercially or systematically, e.g. via an e-mail list or list server);
- present the article at a meeting or conference and to distribute copies of the article to the delegates attending such meeting;
- for your employer, if the article is a ‘work for hire', made within the scope of your employment, your employer may use all or part of the information in the article for other intra-company use (e.g. training);
- retain patent and trademark rights and rights to any process, procedure, or article of manufacture described in the article;
- include the article in full or in part in a thesis or dissertation (provided that this is not to be published commercially);
- use the article or any part thereof in a printed compilation of your works, such as collected writings or lecture notes (subsequent to publication of the article in the journal); and prepare other derivative works, to extend the article into book-length form, or to otherwise re-use portions or excerpts in other works, with full acknowledgement of its original publication in the journal;
- may reproduce or authorize others to reproduce the article, material extracted from the article, or derivative works for the author's personal use or for company use, provided that the source and the copyright notice are indicated.
All copies, print or electronic, or other use of the paper or article must include the appropriate bibliographic citation for the article's publication in the journal.
2. Requests from third parties
Although authors are permitted to re-use all or portions of the article in other works, this does not include granting third-party requests for reprinting, republishing, or other types of re-use.
3. Author Online Use
- Personal Servers. Authors and/or their employers shall have the right to post the accepted version of articles pre-print version of the article, or revised personal version of the final text of the article (to reflect changes made in the peer review and editing process) on their own personal servers or the servers of their institutions or employers without permission from JAKI;
- Classroom or Internal Training Use. An author is expressly permitted to post any portion of the accepted version of his/her own articles on the author's personal web site or the servers of the author's institution or company in connection with the author's teaching, training, or work responsibilities, provided that the appropriate copyright, credit, and reuse notices appear prominently with the posted material. Examples of permitted uses are lecture materials, course packs, e-reserves, conference presentations, or in-house training courses;