FACTORS ASSOCIATED WITH TUBERCULOSIS-DIABETES MELLITUS COMORBIDITY
Faktor-faktor yang Berhubungan dengan Komorbiditas Tuberkulosis-Diabetes Mellitus
Downloads
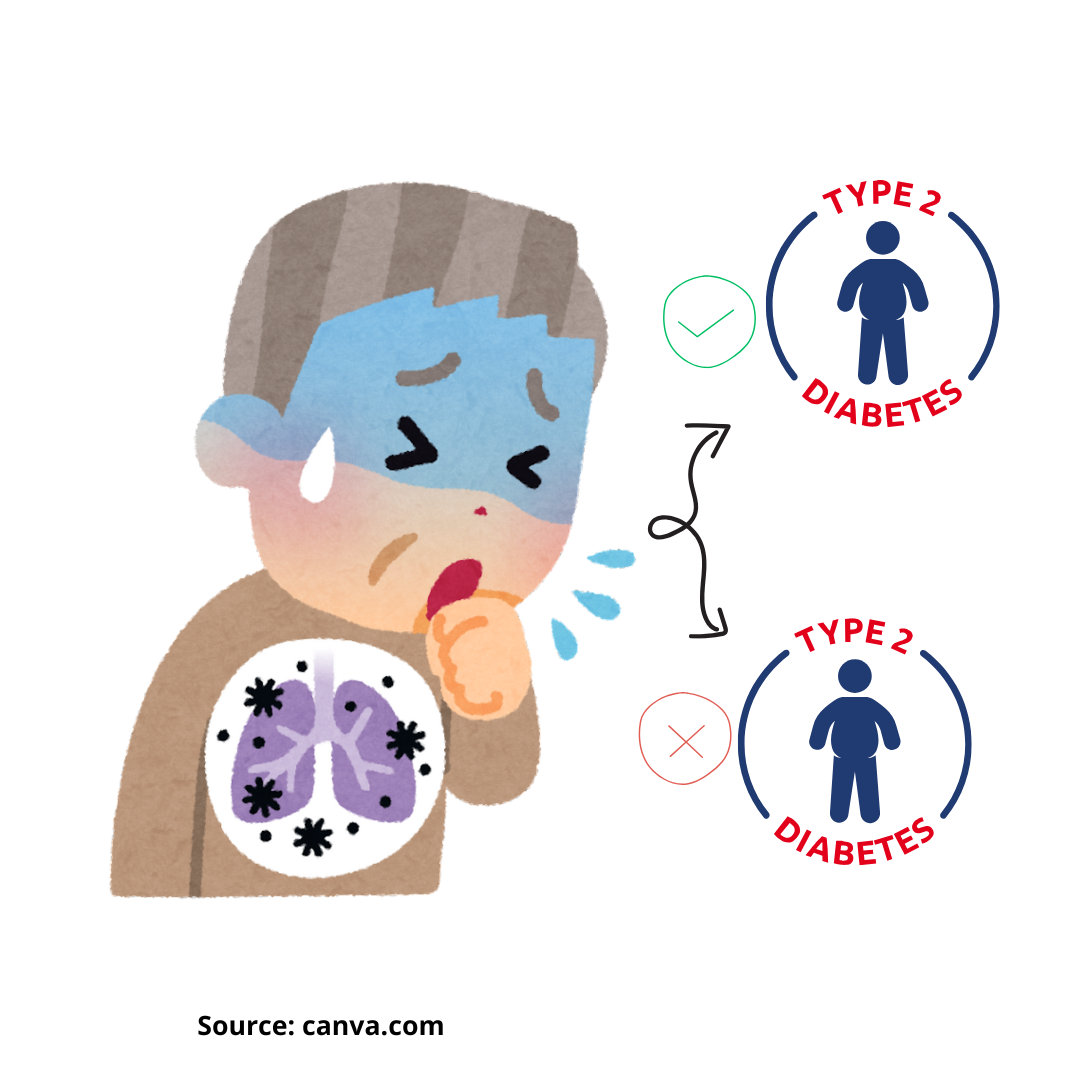
Background: The double burden disease refers to the increase of communicable and non-communicable disease, such as comorbidity tuberculosis (TB) with diabetes mellitus (DM). If not treated properly and managed, tuberculosis can lead to comorbidity with diabetes mellitus. Purpose: This research aims to determine factors associated with tuberculosis-diabetes mellitus comorbidity. Methods: Research design used case-control study, sample cases are TB patients with DM as many as 15 people, while sample control is TB patient without DM as many as 30 people. Independent variables include age, education, occupation, TB severity, body mass index, and quality of life, while the dependent variable is comorbidity TB-DM. The instrument used the World Health Organization’s Quality of Life Brief Version (WHOQOL-BREF). Data analysis was performed utilizing the Chi-Square test and Independent T-test. Results: This study’s findings indicated that the variable age (p= 0.011; OR= 6; 95% CI= 1.39-25.85), education (p=0.03; OR= 4.12; 95% CI= 1.06-16.03), TB severity (p= 0.02; OR= 4.57; 95% CI= 1.18-17.67), and quality of life domains were significantly related to TB-DM with comorbidity: physical (p=0.00; OR=42.25; 95%CI=6.82-261.61), psychological (p=0.03; OR=4; 95% CI=1.07-14.89) and environmental domain (p=0.01; OR=10.54; 95% CI=1.06-105.03). Conclusion: Factors influencing comorbidity between TB-DM include age, education level, TB severity and quality of life. Enhancing immunity in TB patients is essential to reduce the severity of TB and comorbidity of TB-DM, with recommendations for support from family, parents, children, and friends to improve the quality of life for those with TB-DM.
International Diabetes Federation. IDF diatebes atlas 10th edition. 10 th. Diabetes Research and Clinical Practice. 2021.
Soeatmadji DW, Rosandi R, Saraswati MR, Sibarani RP, Tarigan WO. Clinicodemographic profile and outcomes of type 2 Diabetes Mellitus in the Indonesian Cohort of DISCOVER: a 3-year prospective cohort study. J ASEAN Fed Endocr Soc. 2023;38(1):68–74.
WHO. Global tuberculosis report [Internet]. France; 2018.
Ministry of Health of the Republic of Indonesia. Tuberculosis control in Indonesia 2022. 2022.
Khattak M, Rehman A ur, Muqaddas T, Hussain R, Rasool MF, Saleem Z, et al. Tuberculosis (TB) treatment challenges in TB-diabetes comorbid patients: a systematic review and meta-analysis. Ann Med. 2024;56(1).
Ruiz-Grosso P, Cachay R, de la Flor A, Schwalb A, Ugarte-Gil C. Association between tuberculosis and depression on negative outcomes of tuberculosis treatment: A systematic review and meta-analysis. PLoS One. 2020;15(1):e0227472.
Puetri NR, Hadifah Z, Nur A, Hanum S. Comparison of HbA1c levels in patients with TB-DM and TB-non DM. Maj Kedokt Bandung. 2019;51(3):141–6.
Sasmita HY, Prasetyowati I, Wahjudi P. Prevalence and risk factors of diabetes mellitus in tuberculosis patient at Patrang District Indonesia. Indones J Trop Infect Dis. 2019;7(4):79.
Wang Q, Ma A, Han X, Zhao S, Cai J, Ma Y, et al. Prevalence of type 2 diabetes among newly detected pulmonary tuberculosis patients in china: A community based cohort study. PLoS One. 2013;8(12):1–8.
Gil-Santana L, Almeida JL, Oliveira CAM, Hickson LS, Daltro C, Castro S, et al. Diabetes is associated with worse clinical presentation in tuberculosis patients from Brazil: A retrospective cohort study. PLoS One. 2016;11(1):1–13.
Tornu E, Quarcoopome L. Correlates of quality of life among persons living with tuberculosis: A cross-sectional study. PLoS One. 2022;17(11 November):1–13.
Baik Y, Rickman HM, Hanrahan CF, Mmolawa L, Kitonsa PJ, Sewelana T, et al. A clinical score for identifying active tuberculosis while awaiting microbiological results: Development and validation of a multivariable prediction model in sub-Saharan Africa. PLoS Med. 2020;17(11):1–23.
Yadav K, N S, RK Y, CS Gu. Assessment of health-related quality of life among tuberculosis patients with and without diabetes in western region of Nepal. SAARC J Tuberc. 2019;17(2):15–21.
Sartika I, Insani W, Abdulah R. Assessment of health-related quality of life among tuberculosis patients in a public primary care facility in Indonesia. J Glob Infect Dis. 2019;11(3):102–6.
Anasulfalah H, Tamtomo DG, Murti B. Effect of diabetes mellitus comorbidity on mortality risk in tuberculosis patients who received tuberculosis treatment: a meta-analysis. J Epidemiol Public Heal. 2022;7(4):441–53.
Boadu AA, Yeboah-Manu M, Osei-Wusu S, Yeboah-Manu D. Tuberculosis and diabetes mellitus: The complexity of the comorbid interactions. Int J Infect Dis. 2024;146:107140.
Kibirige D, Andia-Biraro I, Olum R, Adakun S, Zawedde-Muyanja S, Sekaggya-Wiltshire C, et al. Tuberculosis and diabetes mellitus comorbidity in an adult Ugandan population. BMC Infect Dis. 2024;24(1):1–9.
Nababan M, Umbul Wahyuni C, Aguslina Siregar F. Factors associated with type 2 Diabetes Mellitus at Adam Malik General Hospital, Medan, Indonesia. J Berk Epidemiol. 2023;11(2):189–97.
Jiang W, Trimawartinah, Rahman FM, Wibowo A, Sanjaya A, Silitonga PII, et al. The co-management of tuberculosis-diabetes co-morbidities in Indonesia under the National Tuberculosis Control Program: results from a cross-sectional study from 2017 to 2019. BMC Public Health. 2022;22(1):1–10.
Anyanwu MO, Ajumobi OO, Afolabi NB, Usman A, Kehinde A. Diabetes mellitus and its associated factors among patients with tuberculosis attending directly observed treatment centres in Oyo State, Nigeria: a cross-sectional evaluation. BMJ Open. 2022;12(4):1–7.
Tenaye L, Mengiste B, Baraki N, Mulu E. Diabetes Mellitus among adult tuberculosis patients attending tuberculosis clinics in Eastern Ethiopia. Biomed Res Int. 2019;2019(Dm).
Tong X, Wang D, Wang H, Liao Y, Song Y, Li Y, et al. Clinical features in pulmonary tuberculosis patients combined with diabetes mellitus in China: An observational study. Clin Respir J. 2021;15(9):1012–8.
Araia ZZ, Mesfin AB, Mebrahtu AH, Tewelde AG, Osman R, Tuumzghi HA. Diabetes mellitus and its associated factors in tuberculosis patients in Maekel region, eritrea: Analytical cross-sectional study. Diabetes, Metab Syndr Obes. 2021;14:515–23.
Cáceres G, Calderon R, Ugarte-gil C. Tuberculosis and comorbidities : treatment challenges in patients with comorbid diabetes mellitus and depression. 2022;1–17.
Liberty P, Liberty M. Type 2 Diabetes Mellitus and pulmonary tuberculosis : literature review of a bidirectional relationship epidemiology of T2DM and pulmonary. Scr SCORE Sci Med J 2023; 5. 2023;5(1):69–75.
Foe-Essomba JR, Kenmoe S, Tchatchouang S, Ebogo-Belobo JT, Mbaga DS, Kengne-Ndé C, et al. Diabetes mellitus and tuberculosis, a systematic review and meta-analysis with sensitivity analysis for studies comparable for confounders. PLoS One. 2021;16(12 December 2021).
Hikmah K, Helda H, Killeen C. Coronavirus-related anxiety with hyperglycemia in type 2 diabetes patients. J Berk Epidemiol. 2022;10(2):111–20.
Ksatriaputra A, Kholis FN, Ngestiningsih D, Bambang Hariyana. Quality of life among tuberculosis patients with and without diabetes mellitus before and after anti-tb drugs administration. J Kedokt Diponegoro. 2020;9(6):475–82.
Febi AR, Manu MK, Mohapatra AK, Praharaj SK, Guddattu V. Psychological stress and health-related quality of life among tuberculosis patients: A prospective cohort study. ERJ Open Res. 2021;7(3).
- Every manuscript submitted to must observe the policy and terms set by the Jurnal Berkala Epidemiologi
- Publication rights to manuscript content published by the Jurnal Berkala Epidemiologi is owned by the journal with the consent and approval of the author(s) concerned. (download copyright agreement)
- Complete texts of electronically published manuscripts can be accessed free of charge if used for educational and research purposes according to copyright regulations.

JBE by Universitas Airlangga is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.























