ESKAPE Pathogens in Hospitalized Patients: A Comprehensive Profiling of Infections and Characteristics at Universitas Airlangga Hospital, Surabaya, Indonesia
Downloads
Highlights
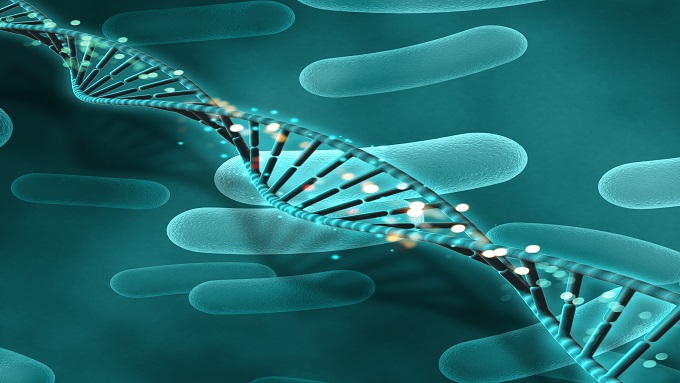
- This study found that ESKAPE pathogenic infections at Universitas Airlangga Hospital were dominated by Gram-negative bacteria, particularly Klebsiella pneumoniae, with sputum as the most commonly collected specimen providing valuable data for infection control strategies.
- Most patients exhibited significant clinical manifestations involving neurological disorders, with the respiratory system being the most affected information that may enhance the effectiveness of patient management in the hospital.
ABSTRACT
Background: Infections pose a significant threat in Indonesia, particularly in healthcare settings where healthcare-associated infections (HAIs) are prevalent. At a hospital in Jakarta, the prevalence of ESKAPE pathogens was reported to be 69.8%. However, detailed data on the infection profiles of these pathogens remain scarce. This underscores the importance of studying ESKAPE pathogenic bacteria to better understand their characteristics. Objective: This study aimed to determine the infection profile of ESKAPE pathogens in hospitalized patients at Universitas Airlangga Hospital, Surabaya, Indonesia in 2022. Material and Method: This descriptive observational study employed a retrospective design using secondary data from non-ICU inpatients at Universitas Airlangga Hospital infected with ESKAPE pathogens in 2022. Total sampling was applied to eligible medical records. Result: The study included 119 specimens from inpatients infected with ESKAPE pathogens that met the inclusion and exclusion criteria. Of these, 78% were Gram-negative bacterial infections, with Klebsiella pneumoniae being the most prevalent (29%). Sputum was the most commonly collected specimen (49%). Most patients were male (57%), aged 56–65 years (29%), and had no comorbidities (46%). Additionally, 63% of patients had used invasive devices during hospitalization. The majority were admitted to low-care inpatient wards. The primary clinical features were neurological complaints (29%) and respiratory disorders (37%), predominantly associated with Klebsiella pneumoniae. Conclusion: ESKAPE infections were primarily caused by Klebsiella pneumoniae, a Gram-negative bacterium, most frequently identified in sputum samples. The predominant clinical manifestations were decreased consciousness and respiratory disorders. Affected patients were mainly male, aged ≥56 years, hospitalized in low-care wards, with a history of invasive device use and no comorbidities.
- Abbas, R. et al., (2024). General Overview of Klebsiella pneumoniae: Epidemiology and the Role of Siderophores in Its Pathogenicity. Biology, 13(78), pp. 3-5. doi:https://doi.org/10.3390/biology13020078.
- Aleem, M. S., Sexton, R., & Akella, J. (2020). Pneumonia In An Immunocompromised Patient. PubMed; StatPearls https://www.ncbi.nlm.nih.gov/books/NBK557843/Publishing.
- Alhumaid, S., Al Mutair, A., Al Alawi, Z., Alzahrani, A.J., Tobaiqy, M., Alresasi, A.M., Bu-Shehab, I., Al-Hadary, I., Alhmeed, N., Alismail, M., Aldera, A.H., AlHbabi, F., Al-Shammari, H., Rabaan, A.A. and Al-Omari, A. (2021). Antimicrobial susceptibility of gram-positive and gram-negative bacteria: a 5-year retrospective analysis at a multi-hospital healthcare system in Saudi Arabia. Annals of Clinical Microbiology and Antimicrobials, 20(1), p.43. doi:https://doi.org/10.1186/s12941-021-00450-x.
- Ashurst, J. V. & Dawson, A., (2023). Klebsiella pneumoniae. StatPearls, pp. 3-5; 26-27 https://pubmed.ncbi.nlm.nih.gov/30085546/.
- Association of Indonesian Clinical Pathology and Laboratory Medicine Specialists, (2018). Surveillance of Multi-Drug Resistant Bacteria and Their Sensitivity to Antibiotics in an Indonesian Hospital, 2018, Daerah Istimewa Yogyakarta: Department of Clinical Pathology and Laboratory Medicine, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada.
- Ayobami, O., Brinkwirth, S., Eckmanns, T. & Markwart, R., (2022). Antibiotic resistance in hospital-acquired ESKAPE infections in low- and lower-middle income countries: a systematic review and meta-analysis. Emerging Microbes & Infection, Volume 11, p. 449. doi:https://doi.org/10.1080/22221751.2022.2030196.
- Bennett, E. E., VanBuren, J., Holubkov, R. & Bratton, S. L., (2018). Presence of Invasive Devices and Risks of Healthcare-Associated Infections and Sepsis. Pediatric Intensive Care, 7(4), pp. 188-195. doi:https://doi.org/10.1055/s-0038-1656535.
- Belete, Y. et al., (2019). Bacterial profile and antibiotics susceptibility pattern of urinary tract infection among children attending Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Infect Drug Resist, 12(83), p. 3575. doi:https://doi.org/10.2147/IDR.S217574.
- Chen, Y.-C., Tsai, I-Ting., Lai, C.-H., Lin, K.-H., & Hsu, Y.-C. (2024). Risk Factors and Outcomes of Community-Acquired Carbapenem-Resistant Klebsiella pneumoniae Infection in Elderly Patients. Antibiotics, 13(3), 282–282. https://doi.org/10.3390/antibiotics13030282.
- Domalaon, R., Idowu, T., Zhanel, G. G. & Schweizer, F., (2018). Antibiotic Hybrids: the Next Generation of Agents and Adjuvants against Gram-Negative Pathogens?. Clinical Microbiology Reviews, 31(2), p. 2. doi:https://doi.org/10.1128/CMR.00077-17.
- Estiningsih, D., Puspitasari, I. & Nuryastuti, T., (2016). Identification of Multidrug-Resistant Organism (MDRO) Infections in Patients Admitted to the Neonatal Intensive Care Unit (NICU) of the Hospital. Jurnal Manajemen dan Pelayanan Farmasi, pp. 243-244. doi:https://doi.org/10.22146/jmpf.351.
- Founou, R. C., Founou, L. L. & Essack, S. Y., (2018). Extended spectrum beta-lactamase mediated resistance in carriage and clinical gram-negative ESKAPE bacteria: a comparative study between a district and tertiary hospital in South Africa. Antimicrobial Resistance & Infection Control, 7(134), p. 4. doi:https://doi.org/10.1186/s13756-018-0423-0.
- Hadiati, D. R., Budayanti, N. S. & Budiman, A., (2018). Prevalence and antimicrobial susceptibility patterns of nosocomial pathogens in Jakarta, Indonesia. Journal of Infection and Public Health, 11(5), pp. 690-693.
- Hamdiyati, K, P. & N., F., (2016). Microbial Patterns and Antibiotic Sensitivity in Patients Admitted to the Intensive Care Unit (ICU) at Sanglah General Hospital, Denpasar, Bali, August-October 2013. E-jurnal medika, Volume 5, pp. 1-6. [online] Unud.ac.id. Available at: https://ojs.unud.ac.id/index.php/eum/article/view/19962/13269.
- Hariati, H., Suza, D. E. & Tarigan, R., (2019). Risk Factors Analysis for Catheter Associated Urinary Tract Infection in Medan, Indonesia. Journal of Medical Sciences, 7(19), p. 3191. doi:https://doi.org/10.3889/oamjms.2019.798.
- Horner, C. et al., (2021). Replacement of Enterococcus faecalis by Enterococcus faecium as the predominanr enterococcus in UK bacteraemias. JAC Antimicrob Resist, pp. 1-6. doi:https://doi.org/10.1093/jacamr/dlab185.
- Izral, M., Laksono, R. M., Isngadi & Basuki, D. R., (2021). The Effect of Using Disposable Breathing Circuits on Bacterial Growth on the Y-Piece of Anesthesia Machines. Jurnal Anestesiologi Indonesia, pp. 24-27. doi:https://doi.org/10.14710/jai.v13i1.16518.
- Karyanti, M. R. & Faisha, K., (2022). Evaluation of Antibiotic Use with the Gyssens Method in Infectious Diseases and Bacterial Sensitivity Patterns in the Pediatric Inpatient Ward at Cipto Mangunkusumo Hospital. Sari Pediatri, 23(6), p. 380. doi:https://doi.org/10.14238/sp23.6.2022.374-82.
- Kemenkes RI, 2021. Regulation of the Indonesian Minister of Health No. 28 of 2021 concerning Guidelines for the Use of Antibiotics, Jakarta: Kemenkes RI. [online] Available at: https://farmalkes.kemkes.go.id/en/unduh/permenkes-28-2021/
- Li, T. et al., (2022). Cigarette Smoking and Peripheral Vascular Disease are Associated with Increasing Risk of ESKAPE Pathogen Infection in Diabetic Foot Ulcers. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, Volume 15, pp. 3271-3281. doi:https://doi.org/10.2147/DMSO.S383701.
- Li, Z. et al., (2021). Pathogenic Characteristics and Risk Factors for ESKAPE Pathogens Infection in Burn Patients. Infection and Drug Resistance, Volume 14, p. 4733. doi:https://doi.org/10.2147/idr.s338627.
- Masoud, S. S. et al., (2022). Extent and Resistance Patterns of ESKAPE Pathogens Isolated in Pus Swabs from Hospitalized Patients. Canadian Journal of Infectious Diseases and Medical Microbiology, p. 4. doi:https://doi.org/10.1155/2022/3511306.
- Mulani, M. S. et al., (2019). Emerging Strategies to Combat ESKAPE Pathogens in the Era of Antimicrobial Resistance: A Review. Frontiers in Microbiology, p. 1. doi:https://doi.org/10.3389/fmicb.2019.00539.
- Paczosa, M. K. & Mecsas, J., (2016). Klebsiella pneumoniae: Going on the Offense with a Strong Defense. Microbiology and Molecular Biology Reviews, 80(3), p. 629. doi:https://doi.org/10.1128/MMBR.00078-15.
- Pandey, R., Mishra, S. K. & Shrestha, A., (2021). Characterisation of ESKAPE Pathogens with Special Reference to Multidrug Resistance and Biofilm Production in a Nepalese Hospital. Infection and Drug Resistance, Volume 14, p. 2204. doi:https://doi.org/10.2147/IDR.S306688.
- Public Health Agency of Canada, (2019). Pathogen Safety Data Sheets: Infectious Substances – Available at: Klebsiella spp.. [Online] Available at: https://www.canada.ca/en/public-health/services/laboratory biosafety-biosecurity/pathogen-safety-data-sheets-risk assessment/klebsiella.html [Accessed 30 Maret 2024].
- Rahmawati, S. A. & Dhamanti, I., (2020). Infection Prevention and Control (IPC) Program in Hospital. Journal of Health Science and Prevention, pp. 23-24. [Online] Available at: http://jurnalfpk.uinsby.ac.id/index.php/jhsp.
- Raudhoh, S. & Pramudiani, D., (2021). Lansia Asik, Lansia Aktif, Lansia Poduktif. MEDIC, 4(1), p. 127. doi:https://doi.org/10.22437/medicaldedication.v4i1.13458.
- Tarina, N. T. I. & Kusuma, S. A. F., (2017). Detection of Klebsiella pneumoniae Bacteria. Farmaka, 15(2), p. 119. doi:https://doi.org/10.24198/jf.v15i2.13173.
- WHO, (2022). Time To Act To Curb Antimicrobial Resistance Now, [Online] Available at:https://www.who.int/indonesia/id/news/detail/12-10-2022time-to-act-to-curb-antimicrobial-resistance-now [2 April 2023].
- Wyres, K. L. & Holt, K. E., (2018). Klebsiella pneumoniae as a key trafficker of drug resistance genes from environmental to clinically important bacteria. Microbiology, Volume 45, pp. 131-134. doi:https://doi.org/10.1016/j.mib.2018.04.004.
- Zhao, J. M. et al., (2022). Klebsiella pneumoniae-related brain abscess and meningitis in adults. Media, 101(2), pp. 1-4. doi:https://doi.org/10.1097/MD.0000000000028415.
Copyright (c) 2025 Dinda Rachma Harlisa, Tri Pudy Asmarawati, Firman Setiawan, Pepy Dwi Endraswari

This work is licensed under a Creative Commons Attribution 4.0 International License.
1. The journal allows the author(s) to hold the copyright of the article without restrictions.
2. The journal allows the author(s) to retain publishing rights without restrictions.
3. The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution 4.0 International License (CC-BY).