Main Article Content
Abstract
Highlights:
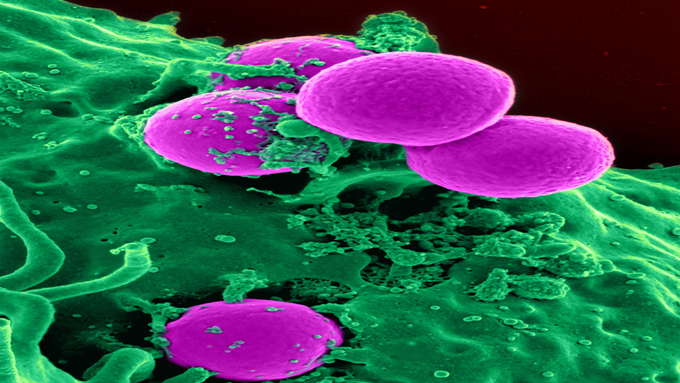
1. The significance of Staphylococcus aureus and coagulase-negative Staphylococcus, which are more likely to infect
immunocompromised patients, needed to be researched in greater depth.
2. Coagulase-negative Staphylococcus was found to form significantly more biofilm than Staphylococcus aureus.
3. Wound care and changing medical devices in immunocompromised patients on a regular basis may provide benefits
to prevent biofilm formation by Staphylococcus spp.
Abstract
Staphylococcus spp. are typically commensal microorganisms that can exist in the human body without causing illness. However, these bacteria have virulence factors, e.g., biofilm formation, that are important to note. Because biofilms shield bacteria from opsonophagocytosis and antimicrobial agents, they can cause persistent or chronic infections. Once they form biofilms, both Staphylococcus aureus and coagulase-negative Staphylococcus (CoNS) can potentially cause incurable infections. This study aimed to compare biofilm formation in Staphylococcus aureus and coagulase-negative Staphylococcus as a guide for the prevention and management of infection, which will maintain and improve the good health of the general population. This was an analytic research with a cross-sectional design. The study began by collecting the samples, identifying the species, and testing the biofilm production with a microtiter plate, which was then analyzed with an enzyme-linked immunosorbent assay (ELISA). Data analysis was conducted using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, N.Y., USA). Comparison tests were conducted using an independent t-test. A value of p<0.05 was used as the cut-off that indicated significance. The total samples were 36 clinical isolates, consisting of 18 Staphylococcus aureus and 18 coagulase-negative Staphylococcus. The specimens consisted of 20 blood samples (55.6%) and 7 wound swabs (19.4%). The biofilm test on the samples showed that 83.3% of the samples produced biofilms. The data revealed that the isolates formed biofilms, with 14 isolates (38.9%) in the strong category, 10 isolates (27.8%) in the moderate category, and each of 6 isolates (16.7%) in the weak and non-existent categories. Both Staphylococcus spp. appeared to have biofilm-forming activity, but coagulase-negative Staphylococcus appeared to be significantly more dominant (p=0.008). Strong biofilm was produced by 61.1% of coagulase-negative Staphylococcus isolates. In conclusion, coagulase-negative Staphylococcus formed a stronger biofilm than Staphylococcus aureus. Its presence as an infection-causing bacteria, particularly in immunocompromised patients, should not be underestimated.
Keywords
Article Details
Copyright (c) 2023 Folia Medica Indonesiana

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
-
Folia Medica Indonesiana is a scientific peer-reviewed article which freely available to be accessed, downloaded, and used for research purposes. Folia Medica Indonesiana (p-ISSN: 2541-1012; e-ISSN: 2528-2018) is licensed under a Creative Commons Attribution 4.0 International License. Manuscripts submitted to Folia Medica Indonesiana are published under the terms of the Creative Commons License. The terms of the license are:
Attribution ” You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
NonCommercial ” You may not use the material for commercial purposes.
ShareAlike ” If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
No additional restrictions ” You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
You are free to :
Share ” copy and redistribute the material in any medium or format.
Adapt ” remix, transform, and build upon the material.

References
- Águila-Arcos S, Álvarez-Rodríguez I, Garaiyurrebaso O, et al (2017). Biofilm-forming clinical staphylococcus isolates harbor horizontal transfer and antibiotic resistance genes. Frontiers in Microbiology. doi: 10.3389/fmicb.2017.02018.
- Banerjee G (2014). Comparative study of biofilm formation in Pseudomonas aeruginosa isolates from patients of lower respiratory tract infection. Journal of Clinical and Diagnostic Research. doi: 10.7860/JCDR/2014/7808.4330.
- Clinical and Laboratory Standards Institute (2022). Performance standards for antimicrobial susceptibility testing, 32nd edn. Clinical and Laboratory Standards Institute, USA. Available at: https://www.nih.org.pk/wpcontent/uploads/2021/ 02/CLSI-2020.pdf.
- Ielapi N, Nicoletti E, Lorè C, et al (2020). The role of biofilm in central venous catheter related bloodstream infections: Evidence-based nursing and review of the literature. Reviews on Recent Clinical Trials 15, 22–27. doi: 10.2174/1574887 114666191018144739.
- Kasperski T, Romaniszyn D, Jachowicz-Matczak E, et al (2023). Extensive drug resistance of strong biofilm-producing acinetobacter baumannii strains isolated from infections and colonization hospitalized patients in Southern Poland. Pathogens 12, 975. doi: 10.3390/pathogens 12080975.
- Kesmodel US (2018). Cross-sectional studies - what are they good for? Acta Obstet Gynecol Scand 97, 388–393. doi: 10.1111/aogs.13331.
- Kwiecinski JM, Jacobsson G, Horswill AR, et al (2019). Biofilm formation by Staphylococcus aureus clinical isolates correlates with the infection type. Infectious Diseases (Auckl) 51, 446–451. doi: 10.1080/23744235.2019.1593499.
- Mahon CR, Lehman DC (2022). Textbook of diagnostic microbiology. Elsevier.
- Mirzaee M, Peerayeh SN, Ghasemian A-M (2014). Detection of icaABCD genes and biofilm formation in clinical isolates of methicillin resistant Staphylococcus aureus. Iranian Journal of Pathology 9, 257–262. Available at: https://ijp.iran path.org/article_7049.html.
- Namvar AE, Asghari B, Ezzatifar F, et al (2013). Detection of the intercellular adhesion gene cluster (ica) in clinical Staphylococcus aureus isolates. GMS hygiene and infection control 8, Doc03. doi: 10.3205/dgkh000203.
- Neopane P, Nepal HP, Shrestha R, et al. (2018). In vitro biofilm formation by Staphylococcus aureus isolated from wounds of hospital-admitted patients and their association with antimicrobial resistance. International Journal of General Medicine 11, 25–32. doi: 10.2147/IJGM.S153268.
- Nourbakhsh F, Namvar AE (2016). Detection of genes involved in biofilm formation in Staphylococcus aureus isolates. GMS Hygiene and Infection Control 11, Doc07. doi: 10.3205/dgkh000267.
- de Oliveira A, Pinheiro-Hubinger L, Pereira VC, et al (2021). Staphylococcal biofilm on the surface of catheters: Electron microscopy evaluation of the inhibition of biofilm growth by RNAIII inhibiting peptide. Antibiotics 10, 879. doi: 10.3390/antibiotics10070879.
- Omidi M, Firoozeh F, Saffari M, et al (2020). Ability of biofilm production and molecular analysis of spa and ica genes among clinical isolates of methicillin-resistant Staphylococcus aureus. BMC Research Notes 13, 19. doi: 10.1186/s13104-020-4885-9.
- Piechota M, Kot B, Frankowska-Maciejewska A, et al (2018). Biofilm formation by methicillin-resistant and methicillin-sensitive Staphylococcus aureus strains from hospitalized patients in Poland. BioMed Research International 2018, 1–7. doi: 10.1155/2018/4657396.
- Pompilio A, Ranalli M, Piccirilli A, et al (2020). Biofilm formation among stenotrophomonas maltophilia isolates has clinical relevance: The ANSELM prospective multicenter study. Microorganisms 9, 49. doi: 10.3390/microorganisms9010049.
- Rasamiravaka T, Labtani Q, Duez P, et al (2015). The formation of biofilms by Pseudomonas aeruginosa : A review of the natural and synthetic compounds interfering with control mechanisms. BioMed Research International 2015, 1–17. doi: 10.1155/2015/759348.
- Riedel S, Hobden JA, Miller S, et al (2019). Jawetz, Melnick, & Adelberg's Medical Microbiology, 28e. McGraw Hill. Available at: https://accessmedicine.mhmedical.com/content.aspxbookid=2629§ionid=217768737.
- Sagar SS, Kumar R, Kaistha SD (2016). Biofilm-an eternalchronicle of bacteria. Indian Journal of Comparative Microbiology, Immunology and Infectious Diseases 37, 45. doi: 10.5958/0974-0147.2016.00010.6.
- Samadi R, Ghalavand Z, Nikmanesh B, et al (2017). Investigation of biofilm formation among methicillin-resistant Staphylococcus aureus isolated from children. Archives of Pediatric Infectious Diseases. doi: 10.5812/pedinfect.61635.
- Seng R, Kitti T, Thummeepak R, et al (2017). Biofilm formation of methicillin-resistant co-agulase negative staphylococci (MR-CoNS) isolated from community and hospital environments ed. de Lencastre H. PLoS One 12, e0184172. doi: 10.1371/journal.pone.0184172.
- Silva-Santana G, Lenzi-Almeida KC, Lopes VGS, et al (2016). Biofilm formation in catheter-related infections by Panton-Valentine leukocidin-producing Staphylococcus aureus. International Microbiology: The Official Journal of The Spanish Society for Microbiology 19, 199–207. doi: 10.2436/20.1501.01.278.
- Singh M, Alsaleem M, Gray CP (2023). Neonatal Sepsis. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24974250.
- Suryanditha PA, Rasita YD, Debora K, et al (2018). icaA/D genes and biofilm formation of methicillin-resistant Staphylococcus aureus in Dr. Soetomo Hospital, Surabaya. Folia Medica Indonesiana 54, 263. doi: 10.20473/fmi.v54i4.10709.
- Tong SYC, Davis JS, Eichenberger E, et al (2015). Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clinical Microbiology Reviews 28, 603–661. doi: 10.1128/CMR.00134-14.
- Torlak E, Korkut E, Uncu AT, et al (2017). Biofilm formation by Staphylococcus aureus isolates from a dental clinic in Konya, Turkey. Journal of Infection and Public Health 10, 809–813. doi: 10.1016/j.jiph.2017.01.004.
- Zheng Y, He L, Asiamah TK, et al (2018). Colonization of medical devices by staphylococci. Environmental Microbiology 20, 3141–3153. doi: 10.1111/1462-2920.14129.
References
Águila-Arcos S, Álvarez-Rodríguez I, Garaiyurrebaso O, et al (2017). Biofilm-forming clinical staphylococcus isolates harbor horizontal transfer and antibiotic resistance genes. Frontiers in Microbiology. doi: 10.3389/fmicb.2017.02018.
Banerjee G (2014). Comparative study of biofilm formation in Pseudomonas aeruginosa isolates from patients of lower respiratory tract infection. Journal of Clinical and Diagnostic Research. doi: 10.7860/JCDR/2014/7808.4330.
Clinical and Laboratory Standards Institute (2022). Performance standards for antimicrobial susceptibility testing, 32nd edn. Clinical and Laboratory Standards Institute, USA. Available at: https://www.nih.org.pk/wpcontent/uploads/2021/ 02/CLSI-2020.pdf.
Ielapi N, Nicoletti E, Lorè C, et al (2020). The role of biofilm in central venous catheter related bloodstream infections: Evidence-based nursing and review of the literature. Reviews on Recent Clinical Trials 15, 22–27. doi: 10.2174/1574887 114666191018144739.
Kasperski T, Romaniszyn D, Jachowicz-Matczak E, et al (2023). Extensive drug resistance of strong biofilm-producing acinetobacter baumannii strains isolated from infections and colonization hospitalized patients in Southern Poland. Pathogens 12, 975. doi: 10.3390/pathogens 12080975.
Kesmodel US (2018). Cross-sectional studies - what are they good for? Acta Obstet Gynecol Scand 97, 388–393. doi: 10.1111/aogs.13331.
Kwiecinski JM, Jacobsson G, Horswill AR, et al (2019). Biofilm formation by Staphylococcus aureus clinical isolates correlates with the infection type. Infectious Diseases (Auckl) 51, 446–451. doi: 10.1080/23744235.2019.1593499.
Mahon CR, Lehman DC (2022). Textbook of diagnostic microbiology. Elsevier.
Mirzaee M, Peerayeh SN, Ghasemian A-M (2014). Detection of icaABCD genes and biofilm formation in clinical isolates of methicillin resistant Staphylococcus aureus. Iranian Journal of Pathology 9, 257–262. Available at: https://ijp.iran path.org/article_7049.html.
Namvar AE, Asghari B, Ezzatifar F, et al (2013). Detection of the intercellular adhesion gene cluster (ica) in clinical Staphylococcus aureus isolates. GMS hygiene and infection control 8, Doc03. doi: 10.3205/dgkh000203.
Neopane P, Nepal HP, Shrestha R, et al. (2018). In vitro biofilm formation by Staphylococcus aureus isolated from wounds of hospital-admitted patients and their association with antimicrobial resistance. International Journal of General Medicine 11, 25–32. doi: 10.2147/IJGM.S153268.
Nourbakhsh F, Namvar AE (2016). Detection of genes involved in biofilm formation in Staphylococcus aureus isolates. GMS Hygiene and Infection Control 11, Doc07. doi: 10.3205/dgkh000267.
de Oliveira A, Pinheiro-Hubinger L, Pereira VC, et al (2021). Staphylococcal biofilm on the surface of catheters: Electron microscopy evaluation of the inhibition of biofilm growth by RNAIII inhibiting peptide. Antibiotics 10, 879. doi: 10.3390/antibiotics10070879.
Omidi M, Firoozeh F, Saffari M, et al (2020). Ability of biofilm production and molecular analysis of spa and ica genes among clinical isolates of methicillin-resistant Staphylococcus aureus. BMC Research Notes 13, 19. doi: 10.1186/s13104-020-4885-9.
Piechota M, Kot B, Frankowska-Maciejewska A, et al (2018). Biofilm formation by methicillin-resistant and methicillin-sensitive Staphylococcus aureus strains from hospitalized patients in Poland. BioMed Research International 2018, 1–7. doi: 10.1155/2018/4657396.
Pompilio A, Ranalli M, Piccirilli A, et al (2020). Biofilm formation among stenotrophomonas maltophilia isolates has clinical relevance: The ANSELM prospective multicenter study. Microorganisms 9, 49. doi: 10.3390/microorganisms9010049.
Rasamiravaka T, Labtani Q, Duez P, et al (2015). The formation of biofilms by Pseudomonas aeruginosa : A review of the natural and synthetic compounds interfering with control mechanisms. BioMed Research International 2015, 1–17. doi: 10.1155/2015/759348.
Riedel S, Hobden JA, Miller S, et al (2019). Jawetz, Melnick, & Adelberg's Medical Microbiology, 28e. McGraw Hill. Available at: https://accessmedicine.mhmedical.com/content.aspxbookid=2629§ionid=217768737.
Sagar SS, Kumar R, Kaistha SD (2016). Biofilm-an eternalchronicle of bacteria. Indian Journal of Comparative Microbiology, Immunology and Infectious Diseases 37, 45. doi: 10.5958/0974-0147.2016.00010.6.
Samadi R, Ghalavand Z, Nikmanesh B, et al (2017). Investigation of biofilm formation among methicillin-resistant Staphylococcus aureus isolated from children. Archives of Pediatric Infectious Diseases. doi: 10.5812/pedinfect.61635.
Seng R, Kitti T, Thummeepak R, et al (2017). Biofilm formation of methicillin-resistant co-agulase negative staphylococci (MR-CoNS) isolated from community and hospital environments ed. de Lencastre H. PLoS One 12, e0184172. doi: 10.1371/journal.pone.0184172.
Silva-Santana G, Lenzi-Almeida KC, Lopes VGS, et al (2016). Biofilm formation in catheter-related infections by Panton-Valentine leukocidin-producing Staphylococcus aureus. International Microbiology: The Official Journal of The Spanish Society for Microbiology 19, 199–207. doi: 10.2436/20.1501.01.278.
Singh M, Alsaleem M, Gray CP (2023). Neonatal Sepsis. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24974250.
Suryanditha PA, Rasita YD, Debora K, et al (2018). icaA/D genes and biofilm formation of methicillin-resistant Staphylococcus aureus in Dr. Soetomo Hospital, Surabaya. Folia Medica Indonesiana 54, 263. doi: 10.20473/fmi.v54i4.10709.
Tong SYC, Davis JS, Eichenberger E, et al (2015). Staphylococcus aureus infections: Epidemiology, pathophysiology, clinical manifestations, and management. Clinical Microbiology Reviews 28, 603–661. doi: 10.1128/CMR.00134-14.
Torlak E, Korkut E, Uncu AT, et al (2017). Biofilm formation by Staphylococcus aureus isolates from a dental clinic in Konya, Turkey. Journal of Infection and Public Health 10, 809–813. doi: 10.1016/j.jiph.2017.01.004.
Zheng Y, He L, Asiamah TK, et al (2018). Colonization of medical devices by staphylococci. Environmental Microbiology 20, 3141–3153. doi: 10.1111/1462-2920.14129.