Spatial Map of Geohelminths Infection in Agricultural Communities and its Contamination in Soil of Jatian Village, Jember Regency

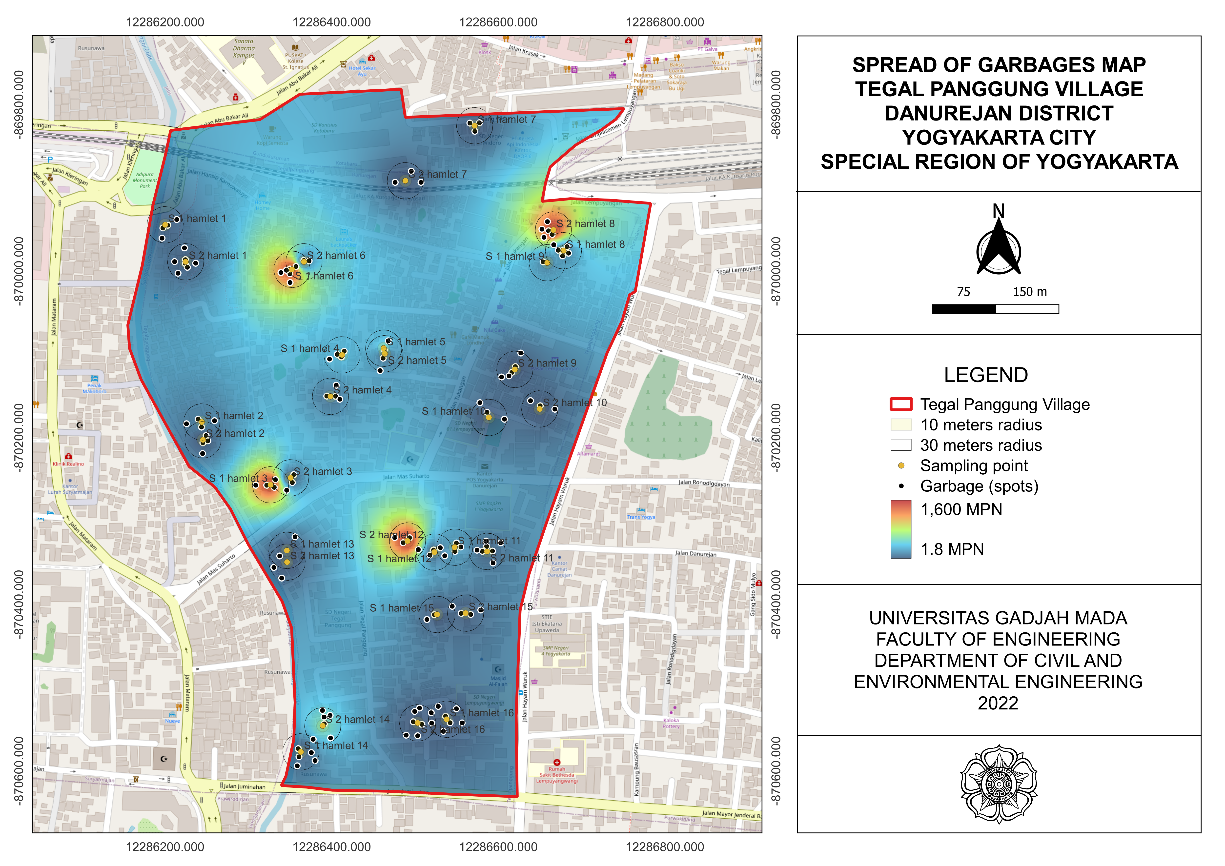
Introduction: Geohelminth infections are a neglected global health problem. Data from the World Health Organization (WHO) in 2020 show that more than 24% of the world population is infected by geohelminths. The condition of the agricultural soil, which tends to be loose and moist, supports the development of the infective form of the geohelminth. This makes agricultural communities susceptible to geohelminth infections. This study aimed to determine a spatial map of geohelminth infection in agricultural communities and its contamination in the soil of Jatian Village, Jember Regency. Methods: This study used an observational analytical design and a spatial analysis approach. Sampling was performed using a random sampling method that included 43 samples. Data were obtained by examining soil and stool samples and the coordinates of the sampling locations. Data were analyzed using spatial analysis. Results and Discussion: The results of this study indicated that the prevalence of geohelminth infection in agricultural communities was 23.3%, and its contamination in the soil was 6.98%. Hookworms caused infections among respondents, and contamination in the ground was caused by Hookworms and Strongyloides stercoralis. Clustering analysis results showed that geohelminth infection formed two secondary clusters. Spatial autocorrelation and buffer analysis showed clustering of geohelminth infections within the buffer range (<100 m), indicating that the infection spreads more easily within the cluster. Conclusion: The spatial map showed the distribution pattern of clustered geohelminth infection cases and their contamination in soil within proximity, thereby increasing the risk of geohelminth transmission.
Gilmour B, Alene KA, Clements ACA. The Prevalence of Soil Transmitted Helminth Infections in Minority Indigenous Populations of South-East Asia and the Western Pacific Region: A Systematic Review and Meta-Analysis. PLoS Neglected Tropical Diseases. 2021;15(11):1–30. https://doi.org/10.1371/journal.pntd.0009890
World Health Organization. Soil-Transmitted Helminth Infections. Geneva: World Health Organization; 2023. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
Bharti B, Bharti S, Khurana S. Worm Infestation: Diagnosis, Treatment and Prevention. Indian Journal of Pediatrics. 2018;85(11):1017–1024. https://doi.org/10.1007/s12098-017-2505-z
Kowalczyk K, KÅ‚apeć T. Contamination of Soil with Eggs of Geohelminths Ascaris spp., Trichuris spp., Toxocara spp. in Poland - Potential Source of Health Risk in Farmers. Annals of Parasitology. 2020;66(4):433–440. https://doi.org/10.17420/ap6604.283
Nugraha TI, Semiarty R, Irawati N. Hubungan Sanitasi Lingkungan dan Personal Hygiene dengan Infeksi Soil Transmitted Helminths (STH) pada Anak Usia Sekolah di Kecamatan Koto Tangah Kota Padang. Jurnal Kesehatan Andalas. 2019;8(3):590–598. https://doi.org/10.25077/jka.v8i3.1046
Baidowi II, Armiyanti Y, Febianti Z, Nurdian Y, Hermansyah B. The Correlation between the Use of Personal Protective Equipment (PPE) and Soil-Transmitted Helminths Infection in the Workers of Kaliputih Plantation Jember Regency. Journal of Agromedicine and Medical Sciemce. 2019;5(2):61–68. https://doi.org/10.19184/ams.v5i2.9625
Saftarina F, Hasan M, Suwandi JF, Syani AY. Kejadian Infeksi Soil-Transmitted Helminth pada Petani. Jurnal Kedokteran Syiah Kuala. 2020;20(3):167–171. https://doi.org/10.24815/jks.v20i3.18732
Apsari PIB, Winianti NW, Arwati H, Dachlan YP. Gambaran Infeksi Soil Transmitted Helminth pada Petani di Desa Gelgel Kabupaten Klungkung. WICAKSANA Jurnal Lingkungan dan Pembangunan. 2020;4(2):21–30. https://doi.org/10.22225/wicaksana.4.2.2020.21-30
Yani I, Putri NLNDD, Abadi MF. The Relationship between Personal Hygiene and Soil Transmitted Helminths in Vegetable Farmers in Gianyar District. Bali Medika Jurnal. 2021;8(3):233–238. https://doi.org/10.36376/bmj.v8i3.162
Prabandari AS, Sari AN, Ferlinda Ahtamagara A, Santo P, Surakarta P. Infeksi Nematoda Usus pada Petani di Kabupaten Sukoharjo Jawa Tengah dan Faktor yang Mempengaruhinya. Indonesian Journal on Medical Science. 2023;10(2):2023.
https://doi.org/10.55181/ijms.v10i2.432
Suparni, Hayunisaq. Hubungan Infeksi Soil Transmitted Helminths (STH) terhadap Karakteristik Masyarakat Lingkungan sekitar Peternakan di Daerah Klumpang Kampung Kecamatan Hamparan Perak. Jurnal Analisa Laboratorium Medis. 2019;1(1):16–23.
Aritonang BNR. Hubungan Personal Higiene dengan Penyakit Cacing (Soil Transmitted Helminth) pada Petani Sayur Kartama Kota Pekanbaru. Jurnal Sains dan Teknologi Laboratorium Medik. 2019;4(2):39–43. https://doi.org/10.52071/jstlm.v4i2.53
Astuti RDI, Ismawati, Rathomi HS. Soil-Transmitted Helminths Contamination on the Yard's Soil of the Public Elementary Schools in Bandung City. Global Medical & Health Communication. 2020;8(3):193–198. https://doi.org/10.29313/gmhc.v8i3.6596
Mahartika RP, Armiyanti Y, Abrori C, Hermansyah B, Nurdian Y. Difference between Location of Soil with Risk of Contamination of Soil-Transmitted Helmints Eggs and Larvae (Observational Study of Coffee Plantation Area in Silo District, Jember Regency). Journal of Agromedicine and Medical Sciences. 2019;5(3):136–140. https://doi.org/10.19184/ams.v5i3.9468
Yaro CA, Kogi E, Luka SA, Yaro CA, Kogi E, Luka SA. Spatial Distribution and Modeling of Soil Transmitted Helminthes Infection in Nigeria. Advances in Infectious Diseases. 2018;8(2):82–107. https://doi.org/10.4236/aid.2018.82010
Anunobi JT, Okoye IC , Aguzie IO , NdukweYE and Okpasuo OJl. Risk of Soil-Transmitted Helminthiasis among Agrarian Communities of Kogi State, Nigeria. Annals of Global Health. 2019;85(1):1–13. https://doi.org/10.5334/aogh.2563
Belay DG, Asratie MH, Gashaw M, Tsega NT, Endalew M, Aragaw FM. Community and Individual Level Determinants and Spatial Distribution of Deworming among Preschool Age Children in Ethiopia: Spatial and Multi-Level Analysis. BMC Public Health. 2022;22(872):1–13. https://doi.org/10.1186/s12889-022-13249-y
Ojja S, Kisaka S, Ediau M, Tuhebwe D, Kisakye AN, Halage AA, et al. Prevalence, Intensity and Factors Associated with Soil-Transmitted Helminths Infections among Preschool-Age Children in Hoima District, Rural Western Uganda. BMC Infectious Diseases. 2018;18(408):1–12. https://doi.org/10.1186/s12879-018-3289-0
Kiiti RW, Omukunda EN, Korir JC. Risk Factors Associated with Helminthic Intestinal Infection in Lurambi Subcounty, Kakamega, Kenya. Journal of Parasitology Research. 2020;2020(8810519):1–9. https://doi.org/10.1155/2020/8810519
Al-Tameemi K, Kabakli R. Ascaris lumbricoides: Epidemiology, Diagnosis, Treatment, and Control. Asian Journal of Pharmaceutical and Clinical Research. 2020;13(4):8–11. https://doi.org/10.22159/ajpcr.2020.v13i4.36930
Gilgen DD, Mascie-Taylor CGNCGN, Rosetta LL. Intestinal Helminth Infections, Anaemia and Labour Productivity of Female Tea Pluckers in Bangladesh. Tropical Medicine & International Health. 2001;6(6):449–457. https://doi.org/10.1046/j.1365-3156.2001.00729.x
Rahmawati ZR, Hermansyah B, Efendi E, Armiyanti Y, Nurdian Y, Utami WS. Association between Personal Hygiene and Incidence of Soil-Transmitted Helminthiasis among Workers at Widodaren Plantation in Jember Regency. Journal of Agromedicine and Medical Sciences (AMS). 2020;6(1):7–13. https://doi.org/10.19184/ams.v6i1.9593
Paniker CKJ, Ghosh S. Paniker's Textbook of Medical Parasitology. London: JP Medical Ltd; 2018. 1–271 p.
Czeresnia JM, Weiss LM. Strongyloides Stercoralis. Lung. 2022;200(2):141–148. https://doi.org/10.1007/s00408-022-00528-z
Goodhead DA, Dirisu CG, Ayenku JE. Observation on Bionomics, Prevalence and Survival Value of Geohelminth in the Rural Communities of Rivers State. African Journal of Biological Sciences. 2022;4(1):48-55. https://doi.org/10.33472/AFJBS.4.1.2022.48-55
Ruliansyah A, Yuliasih Y, Ridwan W, Kusnandar AJ. Analisis Spasial Sebaran Demam Berdarah Dengue di Kota Tasikmalaya Tahun 2011–2015. Aspirator: Jurnal Penelitian Penyakit Tular Vektor. 2017;9(2):85–90. https://dx.doi.org/10.22435/aspirator.v9i2%20Des.6474.85-90
Hernawati R, Ardiansyah MY. Analisis Pola Spasial Penyakit Demam Berdarah Dengue di Kota Bandung Menggunakan Indeks Moran. Rekayasa Hijau Jurnal Teknologi Ramah Lingkungan. 2017;1(3):221–232. https://doi.org/10.26760/jrh.v1i3.1774
Muslimawati NM, Widayani P. Analisis Spasial Penyakit Kecacingan Soil Transmitted Helminth dengan Karakteristik Tanah melalui Pendekatan Geomorfologi di Kabupaten Bantul. Jurnal Bumi Indonesia. 2016;5(1):1–9. https://www.neliti.com/id/publications/223065/analisis-spasial-penyakit-kecacingan-soil-transmitted-helminth-dengan-karakteris#cite
Leta GT, Mekete K, Wuletaw Y, Gebretsadik A, Sime H, Mekasha S, et al. National Mapping of Soil-Transmitted Helminth and Schistosome Infections in Ethiopia. Parasites & Vectors. 2020;13(437):1–13. https://doi.org/10.1186/s13071-020-04317-6
Saputro DR, Widyaningsih P, Kurdi NA, Susanti A. Proporsionalitas Autokorelasi Spasial dengan Indeks Global (Indeks Moran) dan Indeks Lokal (Local Indicator of Spatial Association (LISA)). Prosiding Konferensi Nasional Penelitian Matematika dan Pembelajarannya (KNPMP) III 2018. 2018;3(1):701–710. https://publikasiilmiah.ums.ac.id/handle/11617/10154

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the Jurnal Kesehatan Lingkungan.2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Kesehatan Lingkungan is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
JKESLING by UNAIR is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.