The Impact of Workplace Dust Exposure and Mask Usage on Pulmonary Function in Construction Environments
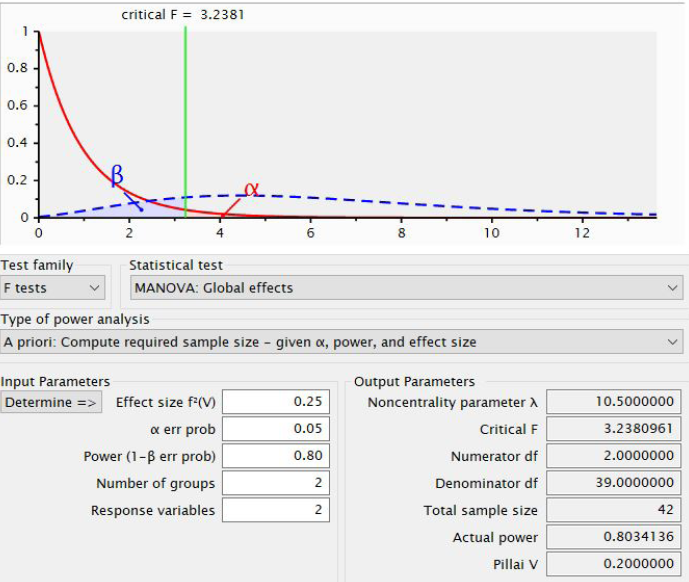
Introduction: The chance of respiratory diseases among workers participating in toll road construction projects is, for example, higher because of non-organic dust. Therefore, this study aims to evaluate the level of lung capacity experienced by the workers by exposing them to dust and wearing masks. Methods: This cross-sectional study investigated toll road projects in Central Java and Yogyakarta and randomly selected workers from different strata of construction companies. The volume Air Sampler estimated dust concentration, while the pulmonary function test included spirometry. All data were analyzed using two-way MANOVA. Results and Discussion: The multivariate analysis of variance showed that workers exposed to dust exceeding the Threshold Limit Value (TLV) had significantly reduced FEV1 and FVC averages (p < 0.001). The averages of FEV1 and FVC increased more considerably in mask users than non-users, indicating mask usage's benefits. The decline in lung function was smaller in mask users, with FEV1 (95% CI: 0.080–0.321) and FVC (95% CI: 0.071–0.404). A reduction in walking distance also demonstrated significance to the decrease in FVC. Conclusion: They found that dust in construction declines lung capacity, but wearing masks provides some protection. However, such impact continues even after stopping wearing masks, thus stressing the importance of correct mask usage and staff training. Subsequent research must investigate dust interaction and various types of masks to enhance Indonesian workers’ health.
Boadu EF, Okeke SR, Boadi C, Bonsu EO, Addo IY. Work-Related Respiratory Health Conditions Among Construction Workers: a Systematic Narrative Review. BMJ Open Respir Res. 2023;10(1):1–10. https://doi.org/10.1136/bmjresp-2023-001736
Norman FZ, Ismail NB, Yasin M, Mohamad M, Muzaini K, Samsudin EZB, et al. The Prevalence and Associated Factors of Suspected Occupational Respiratory Disease Among Construction Workers in Construction Industry in Selangor, Melaka and Pahang State: Secondary Data Analysis of Registry for Occupational Disease Screening (Rods) Database 2023. Res Sq. 2023;4(1):1–24. https://doi.org/10.21203/rs.3.rs-3188958/v1
Keer S, Brooks C, Glass B, McLean D, Harding E, Douwes J. Respiratory Symptoms and Use of Dust-Control Measures in New Zealand Construction Workers – A Cross-Sectional Study. PLoS One. 2022;17(4):1–12. http://dx.doi.org/10.1371/journal.pone.0266668
Kim H, Tae S, Yang J. Calculation Methods of Emission Factors and Emissions of Fugitive Particulate Matter in South Korean Construction Sites. Sustain. 2020;12(23):1–13. https://doi.org/10.3390/su12239802
Indonesian Contractors Association. Sektor Konstruksi Indonesia 2024: Fokus pada Pertumbuhan dan Inovasi. Jakarta: Indonesian Contractors Association; 2024. https://aki.or.id/berita/02/10/2024/243/sektor-konstruksi-indonesia-2024-fokus-pada-pertumbuhan-dan-inovasi/
Murgia N, Akgun M, Blanc P, Costa J, Moitra S, Mu~noz X, et al. The Occupational Burden of Respiratory Diseases, an Update. Pulmonology. 2024;4(3):1–16. https://doi.org/10.1016/j.pulmoe.2024.03.004
Yang K, Wu Y, Chen D, Liu S, Chen R. The Impact of Lung Function on Extra-Pulmonary Diseases and All-Cause Mortality in US Adult Population with and without COPD. Clin Epidemiol. 2020;12(1):997–1005. https://doi.org/10.2147/CLEP.S270599
Whittaker HR, Pimenta JM, Jarvis D, Kiddle SJ, Quint JK. Characteristics Associated with Accelerated Lung Function Decline in a Primary Care Population with Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2020;15(1):3079–3091. https://doi.org/10.2147/COPD.S278981
Kumi L, Jeong J, Jeong J, Lee J. Empirical Analysis of Dust Health Impacts on Construction Workers Considering Work Types. Buildings. 2022;12(8):1-15. https://doi.org/10.3390/buildings12081137
Sheikh A. Global and Regional Burden of Chronic Respiratory Disease in 2016 Arising from Non- Infectious Airborne Occupational Exposures: a Systematic Analysis for The Global Burden of Disease Study 2016. Occup Environ Med. 2020;77(1):142–150. https://doi.org/10.1136/oemed-2019-106013
Alnawaiseh N, El-Gamal FM. The Effect of Cement Dust Exposure on Lung Function Among Cement Factory Workers. Biomed Pharmacol J. 2022;15(4):2061–2068. https://dx.doi.org/10.13005/bpj/2543
Akhter M, Begum M, Akhter S, Datta A. Effects of Exposure to Cement Dust on Lung Function Among Cement Factory Workers. Bangladesh Med Res Counc Bull. 2021;47(2):199–204. https://doi.org/10.3329/bmrcb.v47i2.57780
Mishra AK, Baniya A. Establishing Effective Dust Exposure Limits in Nepal: A Global Imperative for Worker Safety and Health. J UTEC Eng Manag. 2024;2(1):1–12. https://doi.org/10.36344/utecem.2024.v02i01.001
Mariko E, Galey L, Albert M, Langlard B, Garrigou A. Applied Ergotoxicology Methodology in The Construction Sector to Prevent Exposure to Dusts. Occup Med (Chic Ill). 2024;74(1):153-186. https://doi.org/10.1093/occmed/kqae023.0419
Sekhavati E, Yengejeh RJ. Particulate Matter Exposure in Construction Sites is Associated with Health Effects in Workers. Front Public Heal. 2023;11(1):1-7. https://doi.org/10.3389/fpubh.2023.1130620
He W, Jin N, Deng H, Zhao Q, Yuan F, Chen F, et al. Workers’ Occupational Dust Exposure and Pulmonary Function Assessment: Cross-Sectional Study in China. Int J Environ Res Public Health. 2022;19(17):1-11. https://doi.org/10.3390/ijerph191711065
Widiyaristi D, Sunarsih E, Flora R, Windusari Y, Zulkarnain M, Suheryanto S. Risk Factors Affecting Pulmonary Disorders of Workers In Indonesia: Literature Review 2017-2022. J Ilmu Kesehat Masy. 2023;14(3):263–280. https://doi.org/10.26553/jikm.2023.14.3.263-280
Annisa APFD, Achmadi UF. Hubungan Konsentrasi Kadar Debu PM10 dengan Kejadian Gejala ISPA (Infeksi Saluran Pernapasan Akut) Pada Pekerja Proyek Konstruksi X di Depok Tahun 2018. J Nas Kesehat Lingkung Glob. 2020;1(3):272–283. https://doi.org/10.7454/jnklg.v1i3.1018
Zhao Y, Zhao S, Lu J, Dong R, Wang Q, Song G, et al. The Status and Influencing Factors of Lung Ventilation Function in Employees Exposed to Dust in Enterprises of the XPCC, China. Front Public Heal. 2024;12(1):1–18. https://doi.org/10.3389/fpubh.2024.1370765l
Sulaiman NNM, Awang N, Kamaludin NF. Association Between Respirable Dust Exposure and Lung Function Deterioration Among Construction Site Workers. Curr Sci. 2020;119(11):1789–1796. https://doi.org/10.18520/cs/v119/i11/1789-1796
Lestari M, Fujianti P, Nandini RF. Literature Review Dust Exposure and Lung Function Disorders. Respir Sci. 2023;3(3):218–230. https://doi.org/10.36497/respirsci.v3i3.80
Saupin S, Hayati F, Lukman KA, Rahim SSSA, Jeffree MS, Lasimbang HB, et al. Occupational Exposure to Dust and the Relationship with the Respiratory Symptoms, Lung Function among Construction Workers of the University of Malaysia Sabah. Maced J Med Sci. 2022;10(E):1390–1396. https://doi.org/10.3889/oamjms.2022.10186
Gawda A, Majka G, Nowak B, Śróttek M, Walczewska M. Air Particulate Matter SRM 1648a Primes Macrophages to Hyperinflammatory Response After LPS Stimulation. Inflamm Res. 2018;67(1):765–776. https://doi.org/10.1007/s00011-018-1165-4
Hedbrant A, Engström C, Andersson L, Eklund D, Westberg H, Persson A, et al. Occupational Quartz and Particle Exposure Affect Systemic Levels of Inflammatory Markers Related to Inflammasome Activation and Cardiovascular Disease. Environ Heal. 2023;22(25):1–18. https://doi.org/10.1186/s12940-023-00980-1
Zhang Y, Liang J, Cao N, Gao J, Song L, Tang X. Coal Dust Nanoparticles Induced Pulmonary Fibrosis by Promoting Inflammation and Epithelial-Mesenchymal Transition Via the NF-κB/ NLRP3 Pathway Driven by IGF1/ROS-Mediated AKT/GSK3β Signals. Cell Death Discov. 2022;8(500):1–14. https://doi.org/10.1038/s41420-022-01291-z
Goobie GC, Carlsten C, Johannson KA, Khalil N, Marcoux V, Assayag D, et al. Association of Particulate Matter Exposure With Lung Function and Mortality Among Patients With Fibrotic Interstitial Lung Disease. JAMA Intern Med. 2022;182(12):1248–1259. https://https://doi.org/10.1001/jamainternmed.2022.4696
Hou T, Zhu L, Wang Y, Peng L. Oxidative Stress is the Pivot for PM2.5Induced Lung Injury. Food Chem Toxicol. 2024;184(1):114362. https://doi.org/10.1016/j.fct.2023.114362
Barbier E, Carpentier J, Gosset P, Platel A, Alleman LY, Perdrix E. Oxidative Stress and Inflammation Induced by Air Pollution-Derived PM2.5 Persist in the Lungs of Mice After Cessation of Their Sub-Chronic Exposure. Environ Int. 2023;181(1):1-16. https://doi.org/10.1016/j.envint.2023.108248
Handra C, Gurzu I, Chirila M, Ghita I. Silicosis: New Challenges from an Old Inflammatory and Fibrotic Disease. Front Biosci Landmark. 2023;28(5):1–12. https://doi.org/10.31083/j.fbl2805096
Djeghdir S, Peyron A, Sarry G, Leclerc L, Kaouane G, Verhoeven PO, et al. Filtration Efficiency of Medical and Community Face Masks Using Viral and Bacterial Bioaerosols. Sci Rep. 2023;13(1):1–10. https://doi.org/10.1038/s41598-023-34283-9
Ollila HM, Partinen M, Koskela J, Borghi J, Savolainen R, Rotkirch A, et al. Face Masks to Prevent Transmission of Respiratory Infections: Systematic Review and Meta-Analysis of Randomized Controlled Trials on Face Mask Use. PLoS One. 2022;17(12):1–18. http://dx.doi.org/10.1371/journal.pone.0271517
Peters A, Palomo R, Ney H, Lotfinejad N, Zingg W, Parneix P, et al. The COVID-19 Pandemic and N95 Masks: Reusability and Decontamination Methods. Antimicrob Resist Infect Control. 2021;10(1):1–16. https://doi.org/10.1186/s13756-021-00921-y
Guerreiro SFC, Ferreira CAM, Valente JFA, Patrício TMF, Alves NMF, Dias JR. Electrospun-Based Membranes as a Key Tool to Prevent Respiratory Infections. Polymers (Basel). 2022;14(18):1-22. https://doi.org/10.3390/polym14183787
Jonsirivilai B, Torgbo S, Sukyai P. Multifunctional Filter Membrane for Face Mask Using Bacterial Cellulose for Highly Efficient Particulate Matter Removal. Cellulose. 2022;29(11):6205–6218. https://doi.org/10.1007/s10570-022-04641-3
Chen K, Gong Y, Zhao J. Are Facemasks Effective Against Particulate Matter Pollution? Evidence From the Field. J Environ Econ Manage. 2024;125(1):103001. https://doi.org/10.1016/j.jeem.2024.103001
Hellebust S, Wenger J, Sodeau J. Particles at Work and Everywhere Else. Occup Environ Med. 2018;75(2):A111. https://doi.org/10.1136/oemed-2018-ICOHabstracts.316
Gurbaxani BM, Hill AN, Paul P, Prasad P V., Slayton RB. Evaluation of Different Types of Face Masks to Limit the Spread of SARS-CoV-2: a Modeling Study. Sci Rep. 2022;12(1):1–11. https://doi.org/10.1038/s41598-022-11934-x
Choi S, Jeon H, Jang M, Kim H, Shin G, Koo JM, et al. Biodegradable, Efficient, and Breathable Multi-Use Face Mask Filter. Adv Sci. 2021;8(6):1-8. https://doi.org/10.1002/advs.202170028
Kaluarachchi M, Waidyasekara A, Rameezdeen R, Chileshe N. Mitigating Dust Pollution from Construction Activities: A Behavioural Control Perspective. Sustain. 2021;13(16):1–19. https://doi.org/10.3390/su13169005
Ge X, Cui K, Ma H, Zhao S, Meng W, Wang W. Cost-Effectiveness of Comprehensive Preventive Measures for Coal Workers’ Pneumoconiosis in China. BMC Health Serv Res. 2022;22(1):1–10. https://doi.org/10.1186/s12913-022-07654-7
Gao X, Zou H, Chen R, Fang H, Cao Y, Hu Y, et al. RETRACTED: Health Risks and Respiratory Intake of Submicron Particles in the Working Environment: A Case Study. Front Environ Sci. 2022;10(1):1–11. https://doi.org/10.3389/fenvs.2022.1044548
Jate R, Amaral AF, Matteis S De, Lawin H, Mortimer K, Obaseki DO, et al. Association of Respiratory Symptoms and Lung Function with Occupation in the Multinational Burden of Obstructive Lung Disease (BOLD) Study. Eur Respir J. 2023;61(1):1-16. https://doi.org/10.1183/13993003.00469-2022
Moazami TN, Hilt B, Sørås K, Svendsen KVH, Dahlman HJ, Refsnes M, et al. Short-Term Exposure to Stone Minerals Used in Asphalt Affect Lung Function and Promote Pulmonary Inflammation Among Healthy Adults. Scand J Work Environ Heal. 2022;48(5):410–418. https://doi.org/10.5271/sjweh.4023
Seneviratne M, Shankar K, Cantrell P, Nand A. Respirable Crystalline Silica (RCS) Exposure Monitoring, Health Surveillance and Hazard Communication in Preventing Silicosis Among Stone Workers. Occup Environ Med. 2018;75(2):A441. https://doi.org/10.1136/oemed-2018-ICOHabstracts.1256
Asgedom AA. Dust Exposure and Respiratory Health among Selected Factories in Ethiopia: Existing Evidence, Current Gaps and Future Directions. J Respir. 2023;3(2):49–59. https://doi.org/10.3390/jor3020006
Debela M, Kebeta ND, Begosaw AM, Okello G, Azage M. Bagasse Dust Exposure And Chronic Respiratory Symptoms Among Workers in the Metehara and Wonji Sugar Factories in Ethiopia: A longitudinal study design. BMJ Open Respir Res. 2023;10(1):1–13. https://doi.org/10.1136/bmjresp-2022-001511

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the Jurnal Kesehatan Lingkungan.2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Kesehatan Lingkungan is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
JKESLING by UNAIR is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.