Bacterial Colonization on Ventilator Surfaces in the ICU of Government Hospital in Pontianak
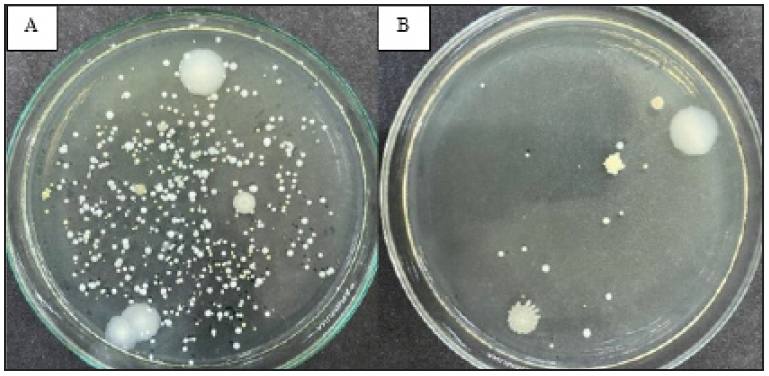
Introduction: Colonization on ventilator surface is causing a risk of pathogenic bacteria transmission, leading to Healthcare-Associated Infections (HAIs). Therefore, this study aimed to determine bacterial colonization on ventilator surface in the Intensive Care Unit (ICU) of Government Hospital in Pontianak. Methods: Two ventilators, designated A and B, were sampled by sterile cotton swabs moistened with NaCl at 7 sampling points, namely power, interface, and control button, as well as screen, handrail, inspiratory port, and expiratory port. Samples were plated in triplication using the spread plate method on tryptone soya agar (TSA) medium and then incubated for 24 hours. The growth colonies were counted, and the morphology was observed macroscopically and microscopically. Results and Discussion: The results showed colonization at all sampling points on both ventilator surfaces. Ventilator A had total average number of colonies of 97, which was significantly higher compared to B with a total average of 7. Gram-negative bacteria (GNB) were observed more than Gram-positive bacteria (GPB) in both ventilators, accounting for 58.75% and 41.25%, respectively. The handrail part showed the highest number of colonies, accounting for 546 and 35 in ventilator A and B, respectively, represent both GNB and GPB but dominated by Gram-Positive coccus. The morphological forms of bacterial cells found were Gram-negative bacillus (GNB), Gram-positive coccus (GPC), Gram-negative coccus (GNC), and Gram-positive bacillus (GPB), with percentages of 37.50%, 27.50%, 21.25%, and 13.75%, respectively. Conclusion: This study showed colonization on the surfaces of two ventilators used in the ICU.
Goh LPW, Marbawi H, Goh SM, Bin Abdul Asis AK. Gansau JA. The Prevalence of Hospital-Acquired Infections in Southeast Asia (1990-2022). J Infect Dev Ctries. 2023;17(02):139–146. https://doi.org/10.3855/jidc.17135
Nimer NA. Nosocomial Infection and Antibiotic-Resistant Threat in the Middle East. Infect Drug Resist. 2022;15(1):631–639. https://doi.org/10.2147/IDR.S351755
Gajdács M, Urbán E, Stájer A, Baráth Z. Antimicrobial Resistance in the Context of the Sustainable Development Goals: A Brief Review. Eur J Investig Health Psychol Educ. 2021;11(1):71–82. https://doi.org/10.3390/ejihpe11010006
Raoofi S, Pashazadeh Kan F, Rafiei S, Hosseinipalangi Z, Noorani Mejareh Z, Khani S, et al. Global prevalence of nosocomial infection: A systematic review and meta-analysis. Kuo YH, editor. PLOS ONE. 2023;18(1):e0274248. https://doi.org/10.1371/journal.pone.0274248
Manoukian S, Stewart S, Graves N, Mason H, Robertson C, Kennedy S, et al. Bed-Days and Costs Associated with The Inpatient Burden of Healthcare-Associated Infection in The UK. J Hosp Infect. 2021;114(1):43–50. https://doi.org/10.1016/j.jhin.2020.12.027
Chakravarthy M, Gore R, Yellappa N, George A, Rangaswamy S, Hosur R, et al. An Analysis of Health Economics Related to Hospital-Associated Infections: A Prospective Case–Control Analysis of 7-Year Data from A Tertiary Referral Corporate Hospital in India. J Patient Saf Infect Control. 2018;6(3):73-77. https://doi.org/10.4103/jpsic.jpsic_20_18
Putra Ritonga E, Silaban NY. Hubungan Fungsi Manajemen Kepala Ruangan dengan Pelaksanaan Pengendalian Infeksi Nosokomial di Rumah Sakit Umum Imelda Pekerja Indonesia Medan. J Ilm Keperawatan IMELDA. 2022;8(1):46–51. https://doi.org/10.52943/jikeperawatan.v8i1.641
Kalagouda R, Kabera B, Muia CK, Ale BM. Hospital Acquired Infections in A Private Paediatric Hospital in Kenya: A Retrospective Cross-Sectional Study. Pan Afr Med J. 2022;41(1):1–14. https://doi.org/10.11604/pamj.2022.41.28.25820
Saba N, Balwan WK. Study of Frequency, Epidemiology of Nosocomial Infections in Healthcare Centres. Saudi J Pathol Microbiol. 2023;8(7):160–166. https://doi.org/10.36348/sjpm.2023.v08i07.001
Ssekitoleko RT, Oshabaheebwa S, Munabi IG, Tusabe MS, Namayega C, Ngabirano BA, et al. The Role Of Medical Equipment in The Spread of Nosocomial Infections: a Cross-Sectional Study in Four Tertiary Public Health Facilities in Uganda. BMC Public Health. 2020;20(1):1561. https://doi.org/10.1186/s12889-020-09662-w
Voidazan S, Albu S, Toth R, Grigorescu B, Rachita A, Moldovan I. Healthcare Associated Infections—A New Pathology in Medical Practice?. Int J Environ Res Public Health. 2020;17(3):760. https://doi.org/10.3390/ijerph17030760
Dai Y, Rao K, Liao Y, Fan H. Analysis on Risk Factors Constituent in 680 Cases of Nosocomial Infection. Wanfang Med 2021;47(14):1904–1907. https://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_cqyx201814016
Pezhman B, Fatemeh R, Amir R, Mahboobeh R, Mohammad F. Nosocomial Infections in An Iranian Educational Hospital: An Evaluation Study of The Iranian Nosocomial Infection Surveillance System. BMC Infect Dis. 2021;21(1):1256. https://doi.org/10.1186/s12879-021-06948-1
Alemu AY, Endalamaw A, Belay DM, Mekonen 14. DK, Birhan BM, Bayih WA. Healthcare-Associated Infection and Its Determinants in Ethiopia: A Systematic Review and Meta-Analysis. PLOS ONE. 2020;15(10):e0241073. https://doi.org/10.1371/journal.pone.0241073
Pettemerides Y, Ghobrial S, Vasilios R, Stelios I. 15. Incidence Rate of Device-Associated, Hospital Acquired Infections in ICUs: A Systematic Review Developed Versus Developing Economies. Int J Caring Sci. 2018;11(3):1914. https://www.internationaljournalofcaringsciences.org/docs/65_iordanou_original_11_3.pdf
Abulhasan YB, Abdullah AA, Shetty SA, Ramadan 16. MA, Yousef W, Mokaddas EM. Health Care-Associated Infections in a Neurocritical Care Unit of a Developing Country. Neurocrit Care. 2020;32(3):836–46. https://doi.org/10.1007/s12028-019-00856-8
Saharman YR, Karuniawati A, Severin JA, Verbrugh 17. HA. Infections and Antimicrobial Resistance in Intensive Care Units in Lower-Middle Income Countries: A Scoping Review. Antimicrob Resist Infect Control. 2021;10(22):1-19. https://doi.org/10.1186/s13756-020-00871-x
Omar AH. Bacterial Contamination on Electronic 18. Surfaces in ICU. Acad J Nawroz Univ. 2024;13(1):658–664. https://doi.org/10.25007/ajnu.v13n1a1889
Papazian L, Klompas M, Luyt CE. Ventilator-19. Associated Pneumonia in Adults: A Narrative Review. Intensive Care Med. 2020;46(5):888–906. https://doi.org/10.1007/s00134-020-05980-0
Wu D, Wu C, Zhang S, Zhong Y. Risk Factors of 20. Ventilator-Associated Pneumonia in Critically Ill Patients. Front Pharmacol. 2019;10(482):1-7. https://doi.org/10.3389/fphar.2019.00482
Gidey K, Gidey MT, Hailu BY, Gebreamlak ZB, 21. Niriayo YL. Clinical and Economic Burden of Healthcare-Associated Infections: A Prospective Cohort Study. Do Prado PR, editor. PLOS ONE. 2023;18(2):e0282141. https://doi.org/10.1371/journal.pone.0282141
Duszynska W, Rosenthal VD, Szczesny A, 22. Zajaczkowska K, Fulek M, Tomaszewski J. Device Associated–Health Care Associated Infections Monitoring, Prevention and Cost Assessment at Intensive Care Unit of University Hospital in Poland (2015–2017). BMC Infect Dis. 2020;20(761):1-10. https://doi.org/10.1186/s12879-020-05482-w
Gonzalez E, Kase J, Getachew F, Cowan M, Scott 23. P, Kyprianou I, et al. Reusable Areas of Clinically Used Ventilators Carry Low Numbers of Aerobic Bacteria. All Res J Biol. 2014;5(4):24–29. http://arjournals.com/index.php/Biol/article/view/106
Sui YS, Wan GH, Chen YW, Ku HL, Li LP, Liu 24. CH, et al. Effectiveness of Bacterial Disinfectants on Surfaces of Mechanical Ventilator Systems. Respir Care. 2012;57(2):250–256. https://doi.org/10.4187/respcare.01180
Ahn Y, Lee UJ, Lee YJ, LiPuma JJ, Hussong D, 25. Marasa B, et al. Oligotrophic Media Compared with a Tryptic Soy Agar or Broth for the Recovery of Burkholderia cepacia Complex from Different Storage Temperatures and Culture Conditions. J Microbiol Biotechnol. 2019;29(10):1495–1505. https://doi.org/10.4014/jmb.1906.06024
Smith F, Lee K, Binnie-McLeod E, Higgins M, 26. Irvine E, Henderson A, et al. Identifying the World Health Organization’s Fifth Moment for Hand Hygiene: Infection Prevention in The Operating Room. J Infect Prev. 2020;21(1):28–34. https://doi.org/10.1177/1757177419879996
Schinas G, Polyzou E, Spernovasilis N, Gogos C, 27. Dimopoulos G, Akinosoglou K. Preventing Multidrug-Resistant Bacterial Transmission in the Intensive Care Unit with a Comprehensive Approach: A Policymaking Manual. Antibiotics. 2023;12(8):1255. https://doi.org/10.3390/antibiotics12081255
Alphons KS, Fortune TV, Haindongo E, Guillaume AY. Bacterial Contamination and Antimicrobial Susceptibility From The Hands of Health Care Workers (HCWs) and Inanimate Surfaces in The Neonatal Intensive Care Unit (NICU) at The Windhoek Central Hospital (WCH). Microbiol Nat. 2020;1(3):83–95. https://doi.org/10.26167/x34y-rn94
Farooq S, Rishi S, Dewani S, Bashir L, Mahnoor M. Drug Resistant Bacterial Contamination of Inanimate Surfaces, Equipment and Health Care Workers in ICU of A Tertiary Care Hospital in North India. Int J Health Sci. 2022;6(S4):4214–4220. https://doi.org/10.53730/ijhs.v6nS4.9227
Dalton K, Rock C, Carroll K, Davis M. One Health in Hospitals: How Understanding The Dynamics of People, Animals, and The Hospital Built-Environment Can Be Used to Better Inform Interventions for Antimicrobial-Resistant Gram-Positive Infections. Antimicrob Resist Infect Control. 2020;9(78):1-17. https://doi.org/10.1186/s13756-020-00737-2
World Health Organization. Care, Cleaning, Disinfection and Sterilization of Respiratory Devices. Geneva: World Health Organization; 2022.
Abubakar Y, Widayat HP, Muzaifa M, Mega FA. Isolasi dan Identifikasi Bakteri Asam Asetat dari Fermentasi Kakao Aceh. J Teknol Pertan Andalas. 2020;24(1):23-28. https://doi.org/10.25077/jtpa.24.1.23-28.2020
Walid A, Novitasari N, Wardany K. Studi Morfologi Koloni Bakteri Udara di Lingkungan Fakultas Tarbiyah dan Tadris Institut Agama Islam Negeri Bengkulu. J IPA Pembelajaran IPA. 2019;3(1):10–14. https://doi.org/10.24815/jipi.v3i1.12974
Singh DM, Rathore P, Gupta S. Study and Isolation of Skin Microflora and their Effects on Human Health. Int J Innov Sci Res Technol. 2018;3(9):592–596. https://ijisrt.com/wp-content/uploads/2018/11/Study-and-Isolation-of-Skin-Microflora-and-their-Effects.pdf
Alhumaid S, Al Mutair A, Al Alawi Z, Alzahrani AJ, Tobaiqy M, Alresasi AM, et al. Antimicrobial Susceptibility of Gram-Positive and Gram-Negative Bacteria: A 5-Year Retrospective Analysis at A Multi-Hospital Healthcare System in Saudi Arabia. Ann Clin Microbiol Antimicrob. 2021;20(43):1-18. https://doi.org/10.1186/s12941-021-00450-x
Tong C, Hu H, Chen G, Li Z, Li A, Zhang J. Disinfectant Resistance in Bacteria: Mechanisms, Spread, and Resolution Strategies. Environ Res. 2021;195(110897):1-9. https://doi.org/10.1016/j.envres.2021.110897
Acsa I, Lilly Caroline B, Philip Njeru N, Lucy Wanjiru N. Preliminary Study on Disinfectant Susceptibility/Resistance Profiles of Bacteria Isolated from Slaughtered Village Free-Range Chickens in Nairobi, Kenya. Int J Microbiol. 2021;1(8877675):1–7. https://doi.org/10.1155/2021/8877675
Breijyeh Z, Jubeh B, Karaman R. Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It. Molecules. 2020;25(6):1340. https://doi.org/10.3390/molecules25061340
Rodríguez-Aguirregabiria M, Asensio-Martín MJ, Nanwani-Nanwani KL. Recurrent Ventilator-Associated Pneumonia Caused by “Difficult to Treat” Resistance Pseudomonas Aeruginosa. Rev Esp Quimioter. 2022;35(Suppl1):117–119. https://doi.org/10.37201/req/s01.25.2022
Adukauskiene D, Ciginskiene A, Adukauskaite A, Koulenti D, Rello J. Clinical Features and Outcomes of Monobacterial and Polybacterial Episodes of Ventilator-Associated Pneumonia Due to Multidrug-Resistant Acinetobacter baumannii. Antibiotics. 2022;11(7):892. https://doi.org/10.3390/antibiotics11070892
Elkammoshi A, Ashur AB, Magrahi HE, Abdulatif A, Almarouq M. The Role of Bacterial Colonization of Ventilator Circuit in Development of Ventilator Associated Pneumonia in ICU of Medical Center Hospital in Tripoli, Libya. Iberoam J Med. 2021;3(2):109–114. https://doi.org/10.53986/ibjm.2021.0019
Nouri F, Karami P, Zarei O, Kosari F, Alikhani MY, Zandkarimi E, et al. Prevalence of Common Nosocomial Infections and Evaluation of Antibiotic Resistance Patterns in Patients with Secondary Infections in Hamadan, Iran. Infect Drug Resist. 2020;13(1):2365–2374. https://doi.org/10.2147/IDR.S259252
Suaya J, Fletcher M, Georgalis L, Aurguedas A, McLaughlin J, Feirerra G, et al. Identification of Streptococcus pneumoniae in Hospital-Acquired Pneumonia in Adults. J Hosp Infect. 2021;108(1):146–157. https://doi.org/10.1016/j.jhin.2020.09.036
Pickens CI, Wunderink RG. Methicillin-Resistant Staphylococcus aureus Hospital-Acquired Pneumonia/Ventilator-Associated Pneumonia. Semin Respir Crit Care Med. 2022;43(02):304–309. https://doi.org/10.1055/s-0041-1740583
Hussain HH, Ibraheem NT, Al-Rubaey NKF, Radhi MM, Hindi NKK, AL-Jubori RHKh. A Review of Airborne Contaminated Microorganisms Associated with Human Diseases. Med J Babylon. 2022;19(2):115–122. https://doi.org/10.4103/MJBL.MJBL_20_22
Wu Y, Wang Y, Yang H, Li Q, Gong X, Zhang G, et al. Resident Bacteria Contribute to Opportunistic Infections of The Respiratory Tract. Peschel A, editor. PLOS Pathog. 2021;17(3):e1009436. https://doi.org/10.1371/journal.ppat.1009436

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the Jurnal Kesehatan Lingkungan.2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Kesehatan Lingkungan is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
JKESLING by UNAIR is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.