Identification of Lead Contamination in the Food Chain and Environment Surrounding Breastfeeding Mothers in Highland Agricultural Areas

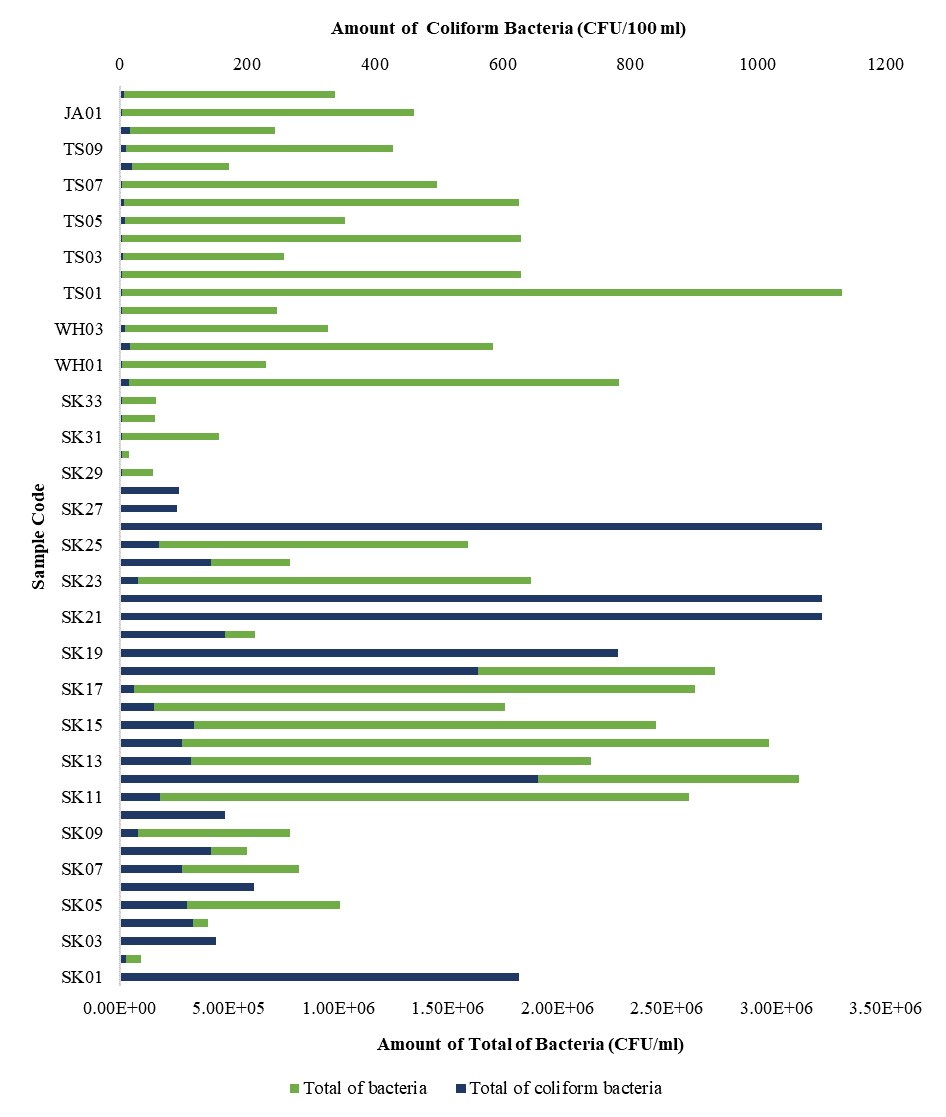
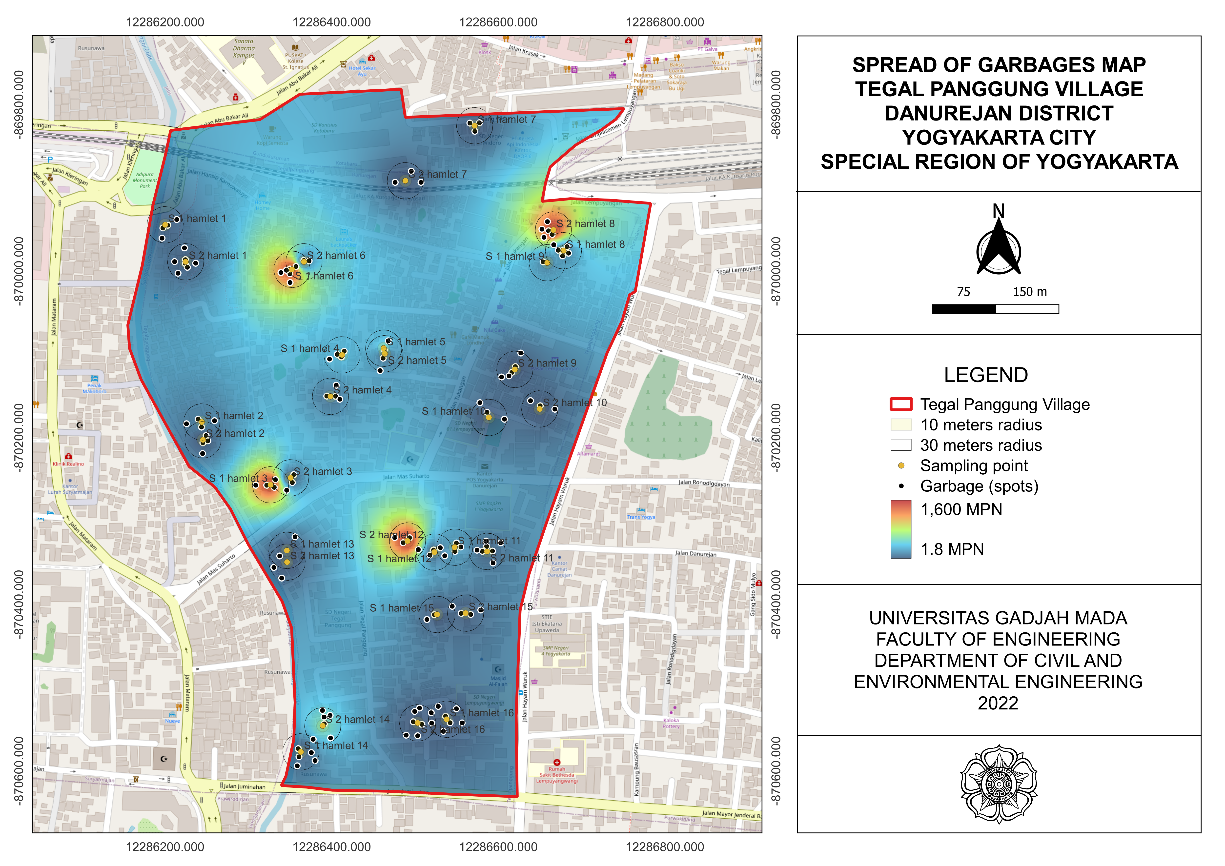
Introduction: Lead in the environment can be more easily absorbed by individuals with nutritional deficiencies, particularly breastfeeding mothers residing in agricultural areas near lead sources. Contaminated breast milk can disrupt infants' growth and development. This study aims to identify lead contaminants in the environment and assess the nutritional status of breastfeeding mothers to provide preventive measures. Methods: This cross-sectional study was conducted in the highland agricultural area of Semarang Regency in October 2021. Environmental samples, including air from agricultural land, settlements, groundwater, and raw food were carried out as environmental samples from 31 breastfeeding mothers. Dietary intake, haemoglobin, MCV, MCH, MCHC, and lead levels in breast milk was carried out. Lead content was analysed using ICP-OES. Geographic information system (GIS) was used to compare spatial distribution lead status levels with identified exposure factors. Results and Discussion: Median age of breastfeeding mothers was 24 years, with 72% being housewives, having a senior high school education. Median age of the infants was 2.5 months, 32% being boys, and 48% were exclusively breastfed. Mean hemoglobin level of the mothers was 13 ± 1.4 g/dL (13.8% was anemic) and median lead level in breast milk was 0.019 ppm. None of the mothers met their recommended macro- and micronutrient intake. Lead content in foods was 0.02-0.180 ppm, groundwater 0.017-0.034 ppm, and air 0-1.56 μg/Nm3 over a three-hours. Conclusion: The environment surrounding breastfeeding mothers contains lead, particularly in the air, and these mother experiences nutritional deficiencies, thereby increasing the risk of lead absorption.
McNeill J, Snider G, Weagle CL, Walsh B, Bissonnette P, Stone E, et al. Large Global Variations in Measured Airborne Metal Concentrations Driven by Anthropogenic Sources. Sci Rep. 2020;10(1):1–12. https://doi.org/10.1038/s41598-020-78789-y
Puspitaloka JA, Wahyuningsih NE, Budiyono. Efektivitas Variasi Ketebalan Arang Aktif Tempurung Kelapa dalam Menyerap Kandungan Logam Berat Timbal (Pb) pada Larutan Pestisida Mengandung Timbal. J Kesehat Masy. 2018;6(6):189–196. https://ejournal3.undip.ac.id/index.php/jkm/article/view/22176/20390
Liu Z, Bai Y, Gao J, Li J. Driving Factors on Accumulation of Cadmium, Lead, Copper, Zinc in Agricultural Soil and Products of the North China Plain. Sci Rep. 2023;13(1):1–13. https://doi.org/10.1038/s41598-023-34688-6
Nabiha PI, Wulandari RA. Health Risk Analysis of Lead Levels (Pb) in Green Leafy Vegetables from Traditional Markets and Supermarket in Semarang City: A Preliminary Study. J Ris Kesehat. 2020;9(1):65–71. http://dx.doi.org/10.31983/jrk.v9i1.5736
Chen T, Dai K, Wu H. Effect of Lead Exposure on Respiratory Health: A Systematic Review and Meta-Analysis. Air Qual Atmos Heal. 2024;17(1):3031-3044. https://link.springer.com/article/10.1007/s11869-024-01619-x
Rahimpoor R, Rostami M, Assari MJ, Mirzaei A, Zare MR. Evaluation of Blood Lead Levels and Their Effects on Hematological Parameters and Renal Function in Iranian Lead Mine Workers. Heal Scope. 2020;9(4):1-10. https://doi.org/10.5812/jhealthscope.95917
Liu ZH, Ai S, Xia Y, Wang HL. Intestinal Toxicity of Pb: Structural and Functional Damages, Effects on Distal Organs and Preventive Strategies. Sci Total Environ. 2024;931(1):1-16. https://doi.org/10.1016/j.scitotenv.2024.172781
Cubello J, Peterson DR, Wang L, Mayer-Proschel M. Maternal Iron Deficiency and Environmental Lead (Pb) Exposure Alter the Predictive Value of Blood Pb Levels on Brain Pb Burden in the Offspring in a Dietary Mouse Model: An Important Consideration for Cumulative Risk in Development. Nutrients. 2023;15(19):1-20. https://www.mdpi.com/2072-6643/15/19/4101
Tatsuta N, Nakai K, Kasanuma Y, Iwai-Shimada M, Sakamoto M, Murata K, et al. Prenatal and Postnatal Lead Exposures and Intellectual Development Among 12-year-old Japanese Children. Environ Res. 2020;189(1):1-9. https://doi.org/10.1016/j.envres.2020.109844
Lin YC, Chang WH, Li TC, Iwata O, Chen HL. Health Risk of Infants Exposed to Lead and Mercury Through Breastfeeding. Expo Heal. 2023;15(1):255–267. https://doi.org/10.1007/s12403-022-00485-1
Ettinger AS, Egan KB, Homa DM, Brown MJ. Blood Lead Levels in U.S. Women of Childbearing Age, 1976–2016. Environ Health Perspect. 2020;128(1):1-9. https://ehp.niehs.nih.gov/doi/full/10.1289/EHP5925
Córdoba-Gamboa L, Vázquez-Salas RA, Romero-Martínez M, Cantoral A, Riojas-Rodríguez H, Bautista-Arredondo S, et al. Lead Exposure Can Affect Early Childhood Development and Could Be Aggravated by Stunted Growth: Perspectives from Mexico. Int J Environ Res Public Health. 2023;20(6):1-17. https://www.mdpi.com/1660-4601/20/6/5174
Asgedom YS, Seifu BL, Mare KU, Asmare ZA, Asebe HA, Kase BF, et al. Levels of Stunting Associated Factors Among Under Five Children in Ethiopia: A Multi-Level Ordinal Logistic Regression Analysis. PLoS One. 2024;19(1):1-13. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0296451
Ashley-Martin J, Dodds L, Arbuckle TE, Lanphear B, Muckle G, Bouchard MF, et al. Blood Metal Levels and Early Childhood Anthropometric Measures in a Cohort of Canadian Children. Environ Res. 2019;179(1):1-8. https://doi.org/10.1016/j.envres.2019.108736
Słota M, Wąsik M, Stołtny T, Machoń-Grecka A, Kasperczyk S. Effects of Environmental and Occupational Lead Toxicity and Its Association with Iron Metabolism. Toxicol Appl Pharmacol. 2022;434(1):1-11. https://doi.org/10.1016/j.taap.2021.115794
Cao Y, Li X, He F, Sun X, Zhang X, Yang T, et al. Comprehensive Screen the Lead and other Toxic Metals in Total Environment from a Coal-gas Industrial City (NW, China): Based on Integrated Source-Specific Risks and Site-Specific Blood Lead Levels of 0–6 Aged Children. Chemosphere. 2021;278(1):1-14. https://doi.org/10.1016/j.chemosphere.2021.130416
Collin S, Baskar A, Geevarghese DM, Ali MNVS, Bahubali P, Choudhary R, et al. Bioaccumulation of Lead (Pb) and Its Effects in Plants: A Review. J Hazard Mater Lett. 2022;3(1):1-8. https://doi.org/10.1016/j.hazl.2022.100064
Amjad M, Khan ZI, Nadeem M, Ahmad K, Shah AA, Gatasheh MK, et al. Accumulation and Translocation of Lead in Vegetables through Intensive Use of Organic Manure and Mineral Fertilizers with Wastewater. Sci Rep. 2024;14(1):1–15. https://doi.org/10.1038/s41598-024-63076-x
Forsyth JE, Saiful Islam M, Parvez SM, Raqib R, Sajjadur Rahman M, Marie Muehe E, et al. Prevalence of Elevated Blood Lead Levels Among Pregnant Women and Sources of Lead Exposure in Rural Bangladesh: A Case Control Study. Environ Res. 2018;166(1):1–9. https://doi.org/10.1016/j.envres.2018.04.019
Kumar S, Islam R, Akash PB, Khan MHR, Proshad R, Karmoker J, et al. Lead (Pb) Contamination in Agricultural Products and Human Health Risk Assessment in Bangladesh. Water, Air, Soil Pollut. 2022;233(7):1-19. https://link.springer.com/article/10.1007/s11270-022-05711-9
Pangestuti DR, Kartini A, Suhartono S, Budiyono B, Lisnawati N, Sulistyawati. Lead Content of Human Milk in Lowland and Highland Agricultural Areas. AIP Conference Proceedings. 2023;2586(1):070012. https://pubs.aip.org/aip/acp/article/2870393
Kartini A, Suhartono S, Budiyono B, Pangestuti DR, Sulistyawati S. Relationship of Breastfeeding Mother’s Lead Levels and Nutritional Status of Infants Aged 0-6 months in Agricultural Areas. Ann Trop Med Public Heal. 2021;24(1):1-9. http://dx.doi.org/10.36295/ASRO.2021.24126
Ministry of Health of Republic Indonesia. Peraturan Menteri Kesehatan No. 28 Tahun 2019 tentang Angka Kecukupan Gizi yang Dianjurkan untuk Masyarakat Indonesia. Jakarta: Ministry of Health of Republic Indonesia; 2019 https://stunting.go.id/kemenkes-permenkes-no-28-tahun-2019-angka-kecukupan-gizi-yang-dianjurkan/
Navya K., Prasad K, Singh BMK. Analysis of Red Blood Cells from Peripheral Blood Smear Images for Anemia Detection: a Methodological Review. Med Biol Eng Comput. 2022;60(1):2445–2462. https://doi.org/10.1007/s11517-022-02614-z
The Indonesian Food and Drug Authority. Peraturan Badan Pengawas Obat dan Makanan Nomor 9 Tahun 2022 Tentang Persyaratan Cemaran Logam Berat dalam Pangan Olahan. Jakarta: BPOM RI Indonesia; 2022 https://standarpangan.pom.go.id/dokumen/peraturan/202x/logam_2022.pdf
National Standardization Agency of Indonesia. SNI 7387:2009. Batas Maksimum Cemaran Logam Berat dalam Pangan. Jakarta: SNI; 2009. https://sertifikasibbia.com/upload/logam_berat.pdf
Sharafi K, Nakhaee S, Azadi NA, Mansouri B, Miri Kermanshahi S, Paknahad M, et al. Human Health Risk Assessment of Potentially Toxic Elements in the Breast Milk Consumed by Infants in Western Iran. Sci Rep. 2023;13(1):1–12. https://doi.org/10.1038/s41598-023-33919-0
CDC. Guidelines for the Identification and Management of Lead Exposure in Pregnant and Lactating Women. Atlanta: Center for Disease Control and Prevention (CDC); 2010. https://stacks.cdc.gov/view/cdc/147837
Cherkani-Hassani A, Slaoui M, Ghanname I, Mojemmi B, Eljaoudi R, Belhaj A, et al. Lead Concentrations in Breast Milk of Moroccan Nursing Mothers and Associated Factors of Exposure: CONTAMILK STUDY. Environ Toxicol Pharmacol. 2021;85(1):1-7. https://doi.org/10.1016/j.etap.2021.103629
Irawati Y, Kusnoputranto H, Achmadi UF, Safrudin A, Sitorus A, Risandi R, et al. Blood Lead Levels and Lead Toxicity in Children Aged 1-5 years of Cinangka Village, Bogor Regency. PLoS One. 2022;17(2):1-13 https://dx.plos.org/10.1371/journal.pone.0264209
Chirinos-Peinado DM, Castro-Bedriñana JI. Lead and Cadmium Blood Levels and Transfer to Milk in Cattle rRared in a Mining Area. Heliyon. 2020;6(3):1-5 https://doi.org/10.1016/j.heliyon.2020.e03579
Shawahna R. Breast Milk to Blood Lead Ratios Among Women from the West Bank of Palestine: a Cross-Sectional Study of Associated Factors. Int Breastfeed J. 2021;16(1):1-13. https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-021-00410-3
Zhao FJ, Tang Z, Song JJ, Huang XY, Wang P. Toxic Metals and Metalloids: Uptake, Transport, Detoxification, Phytoremediation, and Crop Improvement for Safer Food. Mol Plant. 2022;15(1):27–44. https://doi.org/10.1016/j.molp.2021.09.016
Kumar A, Kumar A, Cabral-Pinto M, Chaturvedi AK, Shabnam AA, Subrahmanyam G, et al. Lead Toxicity: Health Hazards, Influence on Food Chain, and Sustainable Remediation Approaches. Int J Environ Res Public Health. 2020;17(7):1-33. https://www.mdpi.com/1660-4601/17/7/2179
Wang M, Liang B, Zhang W, Chen K, Zhang Y, Zhou H, et al. Dietary Lead Exposure and Associated Health Risks in Guangzhou, China. Int J Environ Res Public Health. 2019;16(8):1-16. https://www.mdpi.com/1660-4601/16/8/1417
Padula AM, Rivera-Núñez Z, Barrett ES. Combined Impacts of Prenatal Environmental Exposures and Psychosocial Stress on Offspring Health: Air Pollution and Metals. Curr Env Heal Rep. 2020;7(2):89–100. https://link.springer.com/article/10.1007/s40572-020-00273-6
Dewi T, Martono E, Hanudin E, Harini R. Impact of Agrochemicals Application on Lead and Cadmium Concentrations in Shallot Fields and Their Remediation with Biochar, Compost, and Botanical Pesticides. IOP Conf Ser Earth Environ Sci. 2022;1109(1):1-10. https://iopscience.iop.org/article/10.1088/1755-1315/1109/1/012050
Alengebawy A, Abdelkhalek ST, Qureshi SR, Wang MQ. Heavy Metals and Pesticides Toxicity in Agricultural Soil and Plants: Ecological Risks and Human Health Implications. Toxics. 2021;9(3):1-33. https://www.mdpi.com/2305-6304/9/3/42
World Health Organization. WHO Guideline for Clinical Management of Exposure to Lead. Geneva: World Health Organization; 2021. https://www.ncbi.nlm.nih.gov/books/NBK575284/pdf/Bookshelf_NBK575284.pdf
Obeng A, Roh T, Aggarwal A, Uyasmasi K, Carrillo G. The Contribution of Secondhand Tobacco Smoke to Blood Lead Levels in US Children and Adolescents: a Cross-sectional Analysis of NHANES 2015–2018. BMC Public Health. 2023;23(1):1–9. https://doi.org/10.1186/s12889-023-16005-y

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the Jurnal Kesehatan Lingkungan.2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Kesehatan Lingkungan is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
JKESLING by UNAIR is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.