High Blood Lead Levels as A Risk Factor of Stunting: A Study of Children in Agricultural Areas
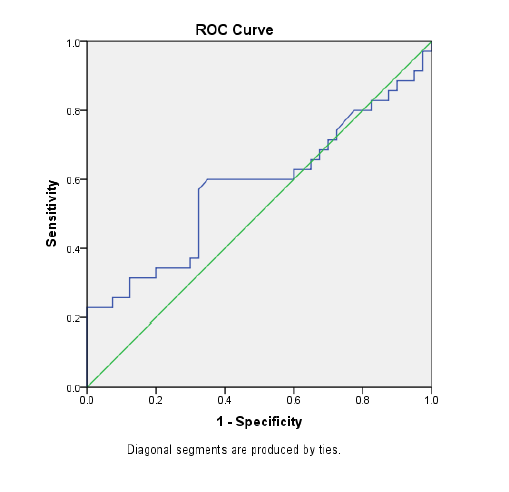
Introduction: The prevalence of stunting among student aged children in Indonesia is relatively high (24.5%). Stunting can threaten the quality of human resources one day. Lead exposure, particularly from pesticides, is thought to disrupt children's development and growth. This study aims to demonstrate that high blood lead levels (BLL) is a risk factor of stunting for children who lives in agricultural areas through the intermediate variable, namely interference with growth hormone (IGF-1). Methods: This study used a case-control design, involving 35 cases (children with HAZ scores of less than -2 SD) and 40 controls (children with HAZ scores of more than -1.5 SD). BLL were measured using the atomic absorption spectrophotometer (AAS) method. Meanwhile, insulin-like growth factor-1 (IGF-1) levels using an ELISA kit (R&D Systems). BLL variables and IGF-1 levels were determined using the receiver operating characteristic (ROC) curve. Results and Discussion: High BLL (>20.44 μg/dL) and low IGF-1 levels (<100 ng/ml) were identified risk factors for stunting in children in agricultural areas with odd ratios (OR) od 2.8 (1.1-7.1) and 3.3 (1.3-8.5) respectively. Meanwhile, a negative correlation was discovered between BLL and IGF-1 levels (p = 0.002, r = -0.356). Conclusion: High lead exposure has been proven to be a risk factor for stunting in children in agricultural areas through the process of interference with the growth hormone, namely IGF-1. Efforts to prevent stunting, especially in agricultural areas, need to take into account exposure to environmental toxicants, including lead from pesticides.
Soliman A, De Sanctis V, Alaaraj N, Ahmed S, Alyafei F, Hamed N, et.al. Early and Long-term Consequences of Nutritional Stunting: From Childhood to Adulthood. Acta Biomed. 2021;92(1):1–12. https://doi.org/10.23750/abm.v92i1.11346
Alaaraj N, Soliman A, Rogol AD. Growth of Malnourished Infants and Children: How is Inflammation Involved?. Expert Review of Endocrinology and Metabolism. 2021;16(5):213–216. https://doi.org/10.1080/17446651.2021.1956903
Vaivada T, Akseer N, Akseer S, Somaskandan A, Stefopulos M, Bhutta ZA. Stunting in Childhood: An Overview of Global Burden, Trends, Determinants, and Drivers of Decline. Am J Clin Nutr. 2020;112(2):777-791. https://doi.org/10.1093/ajcn/nqaa159
Lestari E, Siregar A, Hidayat AK, Yusuf AA. Stunting and Its Association with Education and Cognitive Outcomes in Adulthood: A Longitudinal Study in Indonesia. PLoS One. 2024;19(5):1–18. https://doi.org/10.1371/journal.pone.0295380
UNICEF, WHO, Group WB. Levels and Trends in Child Malnutrition: Key Finding of The 2023 Edition. Asia-Pacific Popul J. 24(2):51–78. https://www.who.int/publications/i/item/9789240073791
World Health Organization. World health statistics 2022 (Monitoring health of the SDGs). Monitoring health of the SDGs. Geneva: World Health Organization; 2022
Alda Fuadiyah Suryono, Kurniawan A, Widyangga PAP, Dewanti MS. Modeling the Stunting Prevalence Rate in Indonesia Using Multi-Predictor Truncated Spline Nonparametric Regression. J Apl Stat Komputasi Stat. 2024;16(1):1–14. https://doi.org/10.34123/jurnalasks.v16i1.719
Ministry of Health of the Republic of Indonesia. Results of the Indonesian Nutrition Status Study Vol. 2. Jakarta: Ministry of Health of the Republic of Indonesia; 2021
Thahir AIA, Li M, Holmes A, Gordon A. Exploring Factors Associated with Stunting in 6-Month-Old Children: A Population-Based Cohort Study in Sulawesi, Indonesia. Nutrients. 2023;15(15):1-17. https://doi.org/10.3390/nu15153420
Balqis B, Rahmadani S, Abadi MY, Rosmanely S, Anwar A, Trisasmita L, et.al. Development of Cross-Sector Collaboration Indicators for Accelerating the Reduction of Stunting in South Sulawesi, Indonesia. J Public Heal Pharm. 2024;4(3):225–237. https://doi.org/10.56338/jphp.v4i3.5924
Shofifah A, Sulistyorini L, Praveena SM. Environmental Sanitation At Home and History of Infection Diseases As Risk Factors for Stunting in Toddlers in Drokilo Village, Kedungadem District, Bojonegoro Regency. J Kesehat Lingkung. 2022;14(4):289–295. https://doi.org/10.20473/jkl.v14i4.2022.289-295
Adi S, Krisnana I, Rahmawati PD, Maghfiroh U. Environmental Factors that Affect the Incidence of Stunting in Under-Five Children: A Literature Review. Pediomaternal Nurs J. 2023;9(1):42–44. https://doi.org/10.20473/pmnj.v9i1.43863
Mutasa K, Tome J, Rukobo S, Govha M, Mushayanembwa P, Matimba FS, et.al. Stunting Status and Exposure to Infection and Inflammation in Early Life Shape Antibacterial Immune Cell Function Among Zimbabwean Children. Front Immunol. 2022;13(13):1–16. https://doi.org/10.3389/fimmu.2022.899296
Kartini A, Subagio HW, Hadisaputro S, Kartasurya MI, Suhartono S, Budiyono B. Pesticide Exposure and Stunting Among Children in Agricultural Areas. Int J Occup Environ Med. 2019;10(1):17–29. https://doi.org/10.15171/ijoem.2019.1428
Widyawati SA, Suhartono S, Mexitalia M, Soejoenoes A. The Relationship Between Pesticide Exposure and Umbilical Serum IGF-1 Levels and Low-Birth Weight: A Case-Control Study in Brebes, Indonesia. Int J Occup Environ Med. 2020;11(1):15–23. https://doi.org/10.15171/ijoem.2020.1809
Alengebawy A, Abdelkhalek ST, Qureshi SR, Wang MQ. Heavy Metals and Pesticides Toxicity in Agricultural Soil and Plants: Ecological Risks and Human Health Implications. Toxics. 2021;9(3):1–34. https://doi.org/10.3390/toxics9030042
Predieri B, Iughetti L, Bernasconi S, Street ME. Endocrine Disrupting Chemicals’ Effects in Children: What We Know and What We Need to Learn?. Int J Mol Sci. 2022;23(19):1-43. https://doi.org/10.3390/ijms231911899
Li N, Cui N, Qiao M, Shen Y, Cheng Y, Song L, et.al. The Effects of Lead Exposure on The Expression of IGF1R, IGFBP3, Aβ40, and Aβ42 in PC12 Cells. J Trace Elem Med Biol. 2022;69(1):1-9. https://doi.org/10.1016/j.jtemb.2021.126877
Liu YY, Milanesi A, Brent GA. Thyroid Hormones. Horm Signal Biol Med Compr Mod Endocrinol. 2020;487–506. https://doi.org/10.1016/b978-0-12-813814-4.00021-3
Rivera-Buse JE, Patajalo-Villalta SJ, Donadi EA, Barbosa F, Magalhães PKR, Maciel LMZ. Impact of Lead Exposure on The Thyroid Glands of Individuals Living in High- or Low-Lead Exposure Areas. Medicine. 2023;102(12):1-5. https://doi.org/10.1097/md.0000000000033292
Wardoyo S, Nurjazuli N, Darundiati YH. Lead Exposure and Stunting Incidents in Children Aged 3–5 Years in Pontianak City, West Kalimantan, Indonesia. Toxicol Anal Clin. 2022;34(2):111–116. https://doi.org/10.1016/j.toxac.2022.02.006
Sakina NA. Blood Lead Levels of Pregnant Women in Agricultural and Coastal Area: A SDG’s Indicator for Health and Pollution in Brebes District. IOP Conf Ser Earth Environ Sci. 2021;940(1):8–13. https://doi.org/10.1088/1755-1315/940/1/012072
Zarmawi R, Haryanto B. The Association of Children’s Blood Lead Levels and Prevalence of Stunting in Tin Mining Area in Indonesia. Ann Glob Heal. 2023;89(1):1–11. https://doi.org/10.5334/aogh.4119
Sastroasmoro S. Fundamentals Clinical Research Methodology. Jakarta: Sagung Seto; 2014.
Olupot-Olupot P, Prevatt N, Engoru C, Nteziyaremye J, Amorut D, Chebet M, et.al. Evaluation of The Diagnostic Accuracy and Cost of Different Methods for The Assessment of Severe Anaemia in Hospitalised Children in Eastern Uganda. Wellcome Open Res. 2019;3(18):1-17. https://doi.org/10.12688/wellcomeopenres.14801.2
Rosalind A Gibson. Principles of Nutritional Assessment. Journal of Human Nutrition and Dietetics. 2006;19(1):72-73. https://doi.org/10.1111/j.1365-277x.2006.00665.x
Brown MJ, Patel P, Nash E, Dikid T, Blanton C, Forsyth JE, et.al. Prevalence of Elevated Blood Lead Levels and Risk Factors Among Children Living in Patna, Bihar, India 2020. PLOS Glob Public Heal. 2022;2(10):1–25. https://doi.org/10.1371/journal.pgph.0000743
Kumar D, Awasthi S, Singh S, Agarwal GG, Pandey AK, Mahdi AA, et.al. Association of Blood Lead Level with Cognitive Performance and General Intelligence of Urban School Children in Ten Cities of India. Clin Epidemiol Glob Heal. 2024;26(1):1-7. https://doi.org/10.1016/j.cegh.2024.101512
Suhartono S, Budiyono B, Dewanti NAY SS. Calcium Supplementation to Reduce Blood Lead Levels in Pregnant Woment (Studies in the Northern Coastel Region Brebes, Indonesia). Ann Trop Med Public Heal. 2021;24(1)1–8. https://www.researchgate.net/publication/351386759_Calcium_supplementation_to_reduce_blood_lead_levels_in_pregnant_womenStudies_in_the_northern_coastal_region_Brebes_Indonesia
Laquatra J. Pesticide Residues and Lead: Neurotoxins in the Home Environment. Int J Eng Technol Informatics. 2023;4(2):1–3. https://doi.org/10.51626/ijeti.2023.04.00055
Haryanti E, Kariada Tri Martuti N. Analysis of Heavy Metal Contamination of Lead (Pb) and Cadmium (Cd) in Red Snapper (Lutjanus sp.) Meat at TPI Kluwut Brebes Life Sci. 2017;3(1):71–76. https://doi.org/10.15294/lifesci.v9i2.47158
Pertiwi S, Setiani O, Suhartono S, Utami R, Rahmiyati E, Yulizar Y. Factors Associated with Blood Lead Levels in Pregnant Women. Avicenna J Heal Res. 2022;5(2):38–46. https://doi.org/10.36419/avicenna.v5i2.680
CDC. CDC Updates Blood Lead Reference Value | Lead | CDC. Atlanta: Centers for Disease Control and Prevention; 2024.
Balali-Mood M, Naseri K, Tahergorabi Z, Khazdair MR, Sadeghi M. Toxic Mechanisms of Five Heavy Metals: Mercury, Lead, Chromium, Cadmium, and Arsenic. Front Pharmacol. 2021;12(1):1–19. https://doi.org/10.3389/fphar.2021.643972
Liu D, Shi Q, Liu C, Sun Q, Zeng X. Effects of Endocrine-Disrupting Heavy Metals on Human Health. Toxics. 2023;11(4):1–8. https://doi.org/10.3390/toxics11040322
Javorac D, Baralić K, Marić Đ, Mandić-Rajčević S, Đukić-Ćosić D, Bulat Z, et.al. Exploring the Endocrine Disrupting Potential of Lead Through Benchmark Modelling – Study in Humans. Environ Pollut. 2023;316(1):1–8. https://doi.org/10.1016/j.envpol.2022.120428
Ernawati F, Syauqy A, Arifin AY, Soekatri MYE, Sandjaja S. Micronutrient Deficiencies and Stunting Were Associated with Socioeconomic Status in Indonesian Children Aged 6–59 Months. Nutrients. 2021;13(6):1–9. https://doi.org/10.3390/nu13061802
Darraj H, Hakami KM, Maghrabi R, Bakri N, Alhazmi M, Names A, et.al. Nutritional Rickets Among Children: A Retrospective Study from Saudi Arabia Pediatr Heal Med Ther. 2023;14(4):301–308. https://doi.org/10.2147/phmt.s425459
Tw SP, Zuniarto AA. Intake of Vitamin A , Calcium , and Zink Between Stunted and Non-Stunted Children in Cirebon. Jurnal Penelitian Pendidikan IPA. 2024; 10(7):4058–4065. https://doi.org/10.29303/jppipa.v10i7.7687
Elisanti AD, Jayanti RD, Amareta DI, Ardianto ET, Wikurendra EA. Macronutrient Intake in Stunted and Non-Stunted Toddlers in Jember, Indonesia. J Public health Res. 2023;12(3):1–6. https://doi.org/10.1177/22799036231197178
Gulick CN, Peddie MC, Jowett T, Hackney AC, Rehrer NJ. Exercise, Dietary Protein, and Combined Effect on IGF-1 HHS Public Access. Int J Sci Res Methodol. 2020;16(3):61–77. https://pmc.ncbi.nlm.nih.gov/articles/PMC7869853/pdf/nihms-1665578.pdf
Budge S, Parker AH, Hutchings PT, Garbutt C. Environmental Enteric Dysfunction and Child Stunting. Nutrition Reviews. 2019;77(4):240–253. https://doi.org/10.1093/nutrit/nuy068
Tickell KD, Atlas HE, Walson JL. Environmental Enteric Dysfunction: A Review of Potential Mechanisms, Consequences and Management Strategies. BMC Medicine. 2019;17(1):1–9. https://doi.org/10.1186/s12916-019-1417-3
Oliveira KJ, Chiamolera MI, Giannocco G, Pazos-Moura CC, Ortiga-Carvalho TM. Thyroid Function Disruptors: From Nature to Chemicals. Journal of Molecular Endocrinology. 2019;62(1):1–19. https://doi.org/10.1530/jme-18-0081
Choi JY, Huh DA, Moon KW. Association Between Blood Lead Levels and Metabolic Syndrome Considering the Effect of the Thyroid-Stimulating Hormone Based on The 2013 Korea National Health and Nutrition Examination Survey. PLoS ONE. 2020;15(1):1–14. https://doi.org/10.1371/journal.pone.0244821
Suhartono S, Kartini A, Budiyono B, Darundiati YH. The Differences In Blood Lead Levels In Women With Gestational Hypertension Or Pre-Eclampsia And Women With Normal Pregnancy (A Study In The North Coast Of Java, Brebes District). J Kesehat Lingkung. 2022;14(1):27–36. https://doi.org/10.20473/jkl.v14i1.2022.27-36
Pardede BK, Utari A, Mexitalia M. Insulin-like Growth Factor-1 and Growth in Infants 0-6 Months of Age. Paediatr Indones Indones. 2021;61(2):89–93. https://doi.org/10.14238/pi61.2.2021.89-93
Garoufalia Z, Papadopetraki A, Karatza E, Vardakostas D, Philippou A, Kouraklis G, et al. Insulin-Like Growth Factor-I and Wound Healing, A Potential Answer to Non-Healing Wounds: A Systematic Review of The Literature and Future Perspectives. Biomed Reports. 2021;15(2):1–5. https://doi.org/10.3892/br.2021.1442
Murray P, Clayton P. Disorders of Growth Hormone in Childhood. Endotext. 202265–70 https://www.ncbi.nlm.nih.gov/books/NBK278971/;
Zhang B, Li H, Wang Y, Li Y, Zhou Z, Hou X, et.al. Mechanism of Autophagy Mediated by IGF-1 Signaling Pathway in The Neurotoxicity of Lead in Pubertal Rats. Ecotoxicol Environ Saf. 2023;251(126):1-9. https://doi.org/10.1016/j.ecoenv.2023.114557
Nijenhuis-Noort EC, Berk KA, Neggers SJCMM, van der Lely AJ. The Fascinating Interplay between Growth Hormone, Insulin-Like Growth Factor-1, and Insulin. Endocrinol Metab. 2024;39(1):83–89. https://doi.org/10.3803/enm.2024.101
Fleisch AF, Burns JS, Williams PL, Lee MM, Sergeyev O, Korrick SA, et.al. Blood Lead Levels and Serum Insulin-Like Growth Factor 1 Concentrations in Peripubertal Boys. Environ Health Perspect. 2013;121(7):854–858. https://doi.org/10.1289/ehp.1206105

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
1. Copyright of all journal manuscripts is held by the Jurnal Kesehatan Lingkungan.2. Formal legal provisions to access digital articles of electronic journal are subject to the provision of the Creative Commons Attribution-ShareAlike license (CC BY-NC-SA), which means that Jurnal Kesehatan Lingkungan is rightful to keep, transfer media/format, manage in the form of databases, maintain, and publish articles.
3. Published manuscripts both printed and electronic are open access for educational, research, and library purposes. Additionally, the editorial board is not responsible for any violations of copyright law.
JKESLING by UNAIR is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.