Predictors of Mortality among Hospitalized Patients with COVID-19 in Egypt-A Retrospective Observational Study

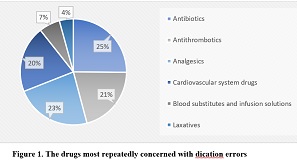
The prediction of mortality and risk stratification of severe coronavirus disease 2019 (Covid-19) offers a rational approach for clinical support, health resource allocation, and implementation of protective interventions to optimize the treatment. Clinicians need these predictors that permit them to elderly patients with Covid-19 rapidly during the pandemic. Investigate demographic features, clinical characteristics, laboratory parameters, and pharmacological treatment received by individuals who died due to Covid-19 that may be predictors of mortality. A retrospective observational study. A single-center cohort in Almaza Fever Egyptian Hospital through three years of the pandemic, 2020, 2021, and 2022. About 194 elderly patients with Covid-19 were attendees of the hospital and died through three years of the pandemic, 2020, 2021, and 2022. A total of 64 cases were in 2020, 94 cases in 2021, and 36 cases in 2022. Main outcome measures: Mortality after a short stay of 9 days evaluated by the area under the curve (AUC), determination of the clinical features, and laboratory measures that may be predictors related to mortality over the three years of the pandemic. Our research found a statistically significant variation between the three years (2020, 2021, and 2022) regarding co-morbidities including IHD, renal and stroke (p-value < 0.05), treatment including Iverzine, chloroquine, remedisvir, and SL (P-value < 0.001), and symptoms including pneumonia status, cytokine storm, dyspnea, cough, anosmia, loss of taste and GIT symptoms (p-value < 0.005). After analysis, there were some predictors, including male sex, age, and hospital stay, that were positively associated with the deterioration of some laboratory measures and biomarkers such as IL-6 with mortality after a short period of stay (9 days) over time. The presented study showed a reliable prediction of mortality over time, so, it plays a crucial role in early patients' identification who are at high risk of death. Therefore, the deteriorated cases should be closely monitored.
INTRODUCTION
The coronavirus disease 2019 (Covid-19) illness, utilizing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pathogenesis, leads to excellent health and societal burdens globally11. The early symptoms noted in Covid-19 patients range from mild to severe22. Mild symptoms include cough, sore throat, fever, dyspnea, anorexia, and fatigue33. A previous study in 552 Chinese hospitals and 30 regions involving 1099 affirmed Covid-19 occurrences. It detected a high percentage of cough (67.7%) and fever (87.9%), and a low percentage of vomiting and diarrhea (less than 5%) occurrence44. The virus may cause severe problems in some patients, such as pneumonia, sepsis, acute respiratory distress syndrome (ARDS), hyperinflammation, neurological symptoms, or multisystem organ failure55.
Our community was significantly impacted by the early Covid-19 pandemic, which seriously affected our everyday routines, financial prudence, and healthcare structures. The adoption of public healthcare programs lowered the rate of infection; however, there is a significant risk that relaxing these regulations will result in the next global epidemic flood, which is already being seen in many nations. The fatality rate of most serious SARS-CoV-2 illnesses transferred to the intensive care (ICU) differs between study results, varying in hospital setting SARS-CoV-2 pneumonia patients (8.1% - 30%) and in intensive care patients (16% - 78%)66. Furthermore, 283 million recorded incidents and 5.41 million reported deaths from Covid-19 on 25 December 2021 in over 237 nations, with a worldwide fatality rate of 1.9% and a sharp everyday rise in the number of occasions77.
Moreover, in the initial Wuhan study, from 41 patients with Covid-19 pneumonia, six (14.6%) patients quickly deteriorated and died due to multiple organ failure;3when the study sample size increased to 99 cases, the deaths were 11 (11.1%)88. In another Wuhan study, 4.3% (six out of 138) was the total mortality in hospitalized Covid-19 pneumonia patients99. Additionally, hospitalization rates, from the first wave in the spring of 2020 until the end of April, increased from 20% to 70%1010.
As of March 2020, numerous investigations on the clinical features of patients with Covid-19 have been publicly released in both minor (n=581111, n=2006) and major studies (n>500071212). However, such research findings found significant differences in patient features that were linked to poor outcomes. Interestingly, these research findings provide only data about clinical findings and predictors on a group level but not about individual patients' prognoses. Furthermore, Covid-19 mortality predictors were defined in multiple types of research involving advanced age1313, male sex1414, and comorbidities1515including coronary artery disease, diabetes mellitus, obesity, malignancy, renal diseases, and hypertension.1616Also, some symptoms included fever1717, cough1717, hemoptysis1313, dyspnea1313, fatigue1717, and loss of consciousness1313, and laboratory measures included high neutrophil-to-lymphocyte ratio (NLR)1313, and high creatinine level1515, lactate dehydrogenase (LDH)1313, direct bilirubin1313and alanine aminotransferase1515, which indicated disease severity, high biomarkers level like serum ferritin, D-dimer15, interleukin-6 (IL-6), procalcitonin (PCT), and C-reactive protein (CRP)14and reinforces these outcomes1515.
Estimation of fatalities and risk stratification provides a logical strategy for clinical support, health care services allotment, and constructing protective methods to maximize treatments available. The effectiveness of special antiviral and directed immunomodulatory treatment is still enigmatic. Additionally, clinical professionals should have a critical need for mortality-leading indicators that enable rapid management of severe (Covid-19) illness1818.
Despite extensive research currently reporting death rates and risk factors worldwide, in-depth research on the clinical traits and consequences of Covid-19 patients in Egypt is still lacking. Therefore, completing the knowledge gap by comprehending the clinical characteristics of Covid-19 can aid in mapping the illness, identifying patients at high risk, and directing healthcare administration in the future. The main goal of this retrospective non-interventional study was to better map and manage the Covid-19 pandemic by examining the clinical characteristics of the virus and locating potential predictors associated with mortality.
MATERIALS AND METHODS
Design and Population is A retrospective observational study was performed to collect data from the medical records of every individual who died from Covid-19 and was an attendee of Almaza Fever Hospital, through three years of pandemic. The study started on January 2023, and the data were collected retrospectively from records starting from 1/1/2020 till the end of 2022.
Inclusion and Exclusion Criteria only patients who died and had complete laboratory results in their records were included in the study. Patients who didn’t have complete records with laboratory results were excluded.
Data collection our research examined retrospective data collected from medical files in Almaza Fever Hospital to assess the clinical consequences of 194 hospitalized elderly patients who died from Covid-19 through three years of the pandemic, 2020, 2021, and 2022. The positive polymerase chain reaction (PCR) was the confirmation test for the diagnosis of Covid-19 illness according to the SARS-CoV-2 virus testing.
Data of some variables were detected, including; sex, age, comorbidities, length of stay in the hospital, pneumonia and other symptoms, laboratory results (neutrophils, d-dimers, hemoglobin, C-reactive protein (CRP), urea, alanine aminotransferase (ALT), aspartate aminotransferase (AST), platelets (PLT), TLC, creatinine, ferritin, and IL-6)
Zhu, N. et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020;382.
Alharbi, Y., Alqahtani, A., Albalawi, O. & Bakouri, M. Epidemiological modeling of COVID-19 in Saudi Arabia: Spread projection, awareness, and impact of treatment. Appl. Sci. 2020;10.
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.
Guan, W. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720.
Alharthy, A. et al. Clinical characteristics and predictors of 28-day mortality in 352 critically ill patients with COVID-19: A retrospective study. J. Epidemiol. Glob. Health 2021;11.
Esfahanian, F., SeyedAlinaghi, S., Janfaza, N. & Tantuoyir, M. M. Predictors of hospital mortality among patients with COVID-19 in Tehran, Iran. SAGE Open Med. 2021;9.
Roser, M., Ritchie, H., Ortiz-Ospina, E. & Hasell, J. Coronavirus disease (COVID-19)–Statistics and research. Our World data 2020.
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395.
Wang, D. et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA - J. Am. Med. Assoc. 2020;323.
Park, M. et al. Determining the communicable period of SARS-CoV-2: A rapid review of the literature, March to September 2020. Eurosurveillance vol. 26 2021. https://doi.org/10.2807/1560-7917.ES.2021.26.14.2001506.
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395.
Docherty, A. et al. Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. medRxiv 2020.
Liang, W. et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern. Med. 2020;180.
Knight, S. R. et al. Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: Development and validation of the 4C Mortality Score. BMJ 2020;370.
et al. Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020. (The Lancet, (S0140673620305663), (101016/S0140-6736(20)30566-3)).
Chauhan, N. K. et al. Predictors of clinical outcomes in adult COVID-19 patients admitted to a tertiary care hospital in India: An analytical cross-sectional study. Acta Biomed. Lancet 2021;92.
Salunke, A. A. et al. A proposed ABCD scoring system for patient’s self assessment and at emergency department with symptoms of COVID-19. Diabetes and Metabolic Syndrome: Clinical Research and Reviews vol. 14 2020. https://doi.org/10.1016/j.dsx.2020.07.053.
Rizo-Téllez, S. A. et al. The neutrophil-to-monocyte ratio and lymphocyte-to-neutrophil ratio at admission predict in-hospital mortality in mexican patients with severe sars-cov-2 infection (Covid-19). Microorganisms. 2020;8.
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395.
Berenguer, J. et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin. Microbiol. Infect. 2020;26.
Kim, L. et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin. Infect. Dis. 2021;72.
Honing, M. L. H., Morrison, P. J., Banga, J. D., Stroes, E. S. G. & Rabelink, T. J. Nitric oxide availability in diabetes mellitus. Diabetes/Metabolism Reviews vol. 14 1998. https://doi.org/10.1002/(SICI)1099-0895(1998090)14:3<241::AID-DMR216>3.0.CO;2-R.
Hermann, M., Flammer, A. & Lüscher, T. F. Nitric oxide in hypertension. Journal of clinical hypertension (Greenwich, Conn.) vol. 8 2006. https://doi.org/10.1111/j.1524-6175.2006.06032.x.
Mehraeen, E. et al. Predictors of mortality in patients with COVID-19–a systematic review. European Journal of Integrative Medicine vol. 40 2020. https://doi.org/10.1016/j.eujim.2020.101226.
Chomistek, A. K. et al. Predictors of critical care, mechanical ventilation, and mortality among hospitalized patients with COVID-19 in an electronic health record database. BMC Infect. Dis. 2022;22.
COVID-19 Treatment Guidelines. https://www.covid19treatmentguidelines.nih.gov/.
Alkundi, A., Mahmoud, I., Musa, A., Naveed, S. & Alshawwaf, M. Clinical characteristics and outcomes of COVID-19 hospitalized patients with diabetes in the United Kingdom: A retrospective single-center study. Diabetes Res. Clin. Pract. 2020;165.
Moledina, S. M. et al. Clinical characteristics and predictors of mortality in patients with COVID-19 infection outside intensive care. Int. J. Gen. Med. 2020;13.
The Sex, Gender and COVID-19 Project | Global Health 50/50. https://globalhealth5050.org/the-sex-gender-and-covid-19-project/.
Griffith, D. M. et al. Men and COVID-19: A biopsychosocial approach to understanding sex differences in mortality and recommendations for practice and policy interventions. Preventing Chronic Disease vol. 17 2020. https://doi.org/10.5888/PCD17.200247.
Albalawi, O. et al. Clinical characteristics and predictors of mortality among COVID-19 patients in Saudi Arabia. J. Infect. Public Health 2021;14.
Tian, W. et al. Predictors of mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis. Journal of Medical Virology vol. 92 2020. https://doi.org/10.1002/jmv.26050.
Tang, N., Li, D., Wang, X. & Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18.
Copyright (c) 2024 Mohamed Abdel-Salam Elgohary, Mostafa Mahmoud Elnakib, Mohamed G Seadawy, Mohamed Emam Mohamed5, dina elaraby, Amany Ahmad Ibrahim, Osama Hasan Bekheet, Ashraf Ibrahim Zaki, Mahmoud Zeinhom Abdelfattah, Hesham Mosaad Sheshtawy, Marina Raouf Abdelmessih Saleeb, Nouran Ameen Hamza, Nashwa Naguib Omar, Ahmed Mahmoud ElShafei , Jacklin Samir kamal6

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.