The Relationship Between Anemia in Pregnant Women and The Incidence of Preeclampsia in Indonesia : A Systematic Review

Preeclampsia is the biggest cause of morbidity and mortality worldwide and the second most common cause of maternal death in Indonesia. One of the highest risk factors for preeclampsia is anemia, so this study aimed to conduct a systematic review of the relationship between anemia in pregnant women and the incidence of preeclampsia. This research was an analytic type with a systematic review method from previous research with an observational case-control approach design with secondary data sources. The data were obtained from the results of previous research with a literature time limit of the last 5 years (2018–2022). This study used databases from Google Scholar, Pubmed, ScienceDirect, Garuda, and Summon Universitas Airlangga. The search yielded 2161 studies; after eliminating 439 duplicates, 1732 remained. After exclusion based on titles and abstracts, 36 studies remained, which were screened in full text. Finally, 8 studies were eligible and included in the review. Four studies showed a relationship between anemia in pregnant women and the incidence of preeclampsia, while four other studies showed no relationship. The prevalence of anemia in pregnant women in Indonesia ranges from 13.27% to 80.8%, with an average of 44.1%. Ages at risk for preeclampsia in Indonesia are pregnant women aged <20 years and >35 years. There is a relationship between anemia in pregnant women and the incidence of preeclampsia in Indonesia. Therefore, anemia can be a risk factor for preeclampsia.
INTRODUCTION
Preeclampsia is a major cause of maternal and perinatal morbidity and mortality in the world11. Ten to 15% of maternal deaths are related to preeclampsia and eclampsia22. Based on data from the WHO, the incidence of preeclampsia ranged from 0.51% - 38.4% in 201733. The incidence of preeclampsia in Indonesia reaches 3–10% of all pregnancies44. The etiology of preeclampsia is not well known yet, but several risk factors can predispose to preeclampsia, including genetic factors and medical conditions in pregnant women such as diabetes, kidney disease, obesity, and anemia. Other risk factors are age >30 years, previous history of preeclampsia, s pregnancies55.
Twenty-six percent of pregnant women with preeclampsia are known to have anemia as a risk factor66. One of the risk factors for preeclampsia is anemia, a condition that is quite common in pregnant women. The prevalence of anemia in pregnant women globally is 36.5%77, while the prevalence of anemia in Indonesia itself is still high at 48.9% in 2018, where there is 11.8% increase in prevalence from 37.1% in 201388.
In one study in Indonesia, it was stated that there was a relationship between anemia in pregnancy and the incidence of preeclampsia. The possibility of preeclampsia was 2.7 times higher in pregnant women with anemia than in those who were not anemic99, while contradictory results were found in another study that stated that anemia and the incidence of preeclampsia were not related1010.
Based on the illustration above, the prevalence of preeclampsia and anemia in Indonesia is still high and concerning. As there were differences in results between previous studies, the study aimed to review systematically the relationship between anemia in pregnant women and the incidence of preeclampsia in Indonesia.
MATERIALS AND METHODS
This systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We systematically searched the Google Scholar, PubMed, ScienceDirect, Garuda, and Summon UNAIR databases. The key terms searched were “preeclampsia”, “anemia”, “pregnant women”, and “Indonesia”.
We retrieved all the literature from 2017 until 2022. The included literature were those with research subjects of pregnant women tested for anemia during their pregnancy, the literature were written in English and Indonesian with qualitative methods of research located in Indonesia. We excluded literature that used qualitative methods and could not be retrieved with full access. The extracted data from all the retrieved literature was collected and tabulated using Rayyan and Microsoft Excel to be further analyzed.
RESULTS
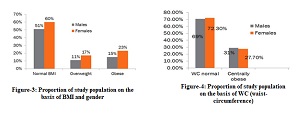
Guidelines for searching data in this study were based on the PRISMA flowchart (Figure 1). This guide was divided into three phases, starting with identification, screening, and included studies. Identification of study searches was based on keywords: anemia, pregnant women, preeclampsia, and Indonesia into databases. The literature search used 5 databases with a total of 2,161 literature collected. Before the screening, 429 pieces of literature were collected and erased due to duplication. The initial stage of screening was to construct a study with an appropriate title and abstract. After screening the titles and the abstracts, 1,696 pieces of literature were excluded. Literature that passed the screening—as many as 36 pieces—were accessed in full text to assess the feasibility of literature based on inclusion and exclusion criteria. Two pieces of literature were found using a cross-sectional study design, one literature had an inappropriate sample, and 25 pieces of literature that did not meet the inclusion criteria were excluded. In this literature research, eight literature were finally selected. The assessment of the quality of the literature in this study used JBI Critical Appraisal Tools.
Figure 1.Literatures Search Result with PRISMA chart (2020)
Table 1 contains the general characteristics of the literature that used in this systematic review, including the name of the author, the title of the study, the location of the study, the year of the study, and the study design. Table 2 contains the characteristics of the study subjects (maternal age, gestational age, number of gravidas) and the number of subjects with anemia and preeclampsia. The literature were obtained from 2018 – 2022. The research locations were spread across several regions of Indonesia. All literature used a case-control research design.
Table 3 contains four literature published from 2018 to 2022 that showed a relationship between anemia in pregnancy and the incidence of preeclampsia with a p-value less than 0.059,11,12,169111216. On the contrary, there were four literature that showed an insignificant relationship between anemia in pregnancy and the incidence of preeclampsia with a p-value greater than 0.0513-15,1713141517.
Table 4 shows the data on pregnant women with anemia with the incidence of preeclampsia and non-preeclampsia. The classification of anemia in this study was based on the level of hemoglobin (Hb) below 11g/dL. Table 4 shows that four literature reveal that women with anemia in pregnancy are experiencing preeclampsia.
Author | Title | Location | Year |
Ameliai, E. & Sutarno, M. | The influence of anemia in the event of preeclampsia in maternal | Banten Regional Police Bhayangkara Hospital | 2021 |
Hamzah, S., et al. | Antenatal care parameters that are the risk factors in the event of preeclampsia in primigravida | HM. Djafar Harun dan Benyamin Guluh Regional Public Hospital, Southeast Sulawesi | 2021 |
Nanda, A. & Semarawisma, A. | The association between anemia |
Andriani, C., Lipoeto, N. I. & Indra Utama, B. Hubungan Indeks Massa Tubuh dengan Kejadian Preeklampsia di RSUP Dr. M. Djamil Padang. J. Kesehat. Andalas 5, 173–178 (2016).
Gustirini, R. Calcium Supplementation In Pregnant Women To Reduce Preeclampsia Incidence In Developing Countries. J. Kebidanan 8(2), 151–160 (2019).
Aulya, Y., Silawati, V. & Safitri, W. Analisis Preeklampsia Ibu Hamil pada Masa Pandemi Covid-19 di Puskesmas Sepatan Kabupaten Tangerang Tahun 2021. J. Akad. Baiturrahim Jambi 10, 375 (2021).
Bardja, S. Faktor risiko terjadinya preeklampsia berat/eklampsia pada ibu hamil. Embrio J. Kebidanan (2020).
Mareg, M., Molla, A., Dires, S., Mamo, Z. B. & Hagos, B. Determinants of preeclampsia among pregnant mothers attending antenatal care (ANC) and delivery service in Gedeo Zone, Southern Ethiopia: Case control-study. Int. J. Womens. Health 12, 567–575 (2020).
Aldika Akbar, M. I. et al. The massive problem of preeclampsia in indonesia: In need of a redesigned national health care system. Pregnancy Hypertens. 13, S16 (2018).
World Health Organization. Anemia. (2023).
RI, K. K. Hasil Riset Kesehatan Dasar (Riskesda). (2018).
Pradipta, F., Hernayanti, M. & Yumei, M. Hubungan Anemia Dalam Kehamilan Dengan Kejadian Preeklampsia Ibu Bersalin di RSUD Kota Yogyakarta Tahun 2017 – 2018. (2019).
Susanti, D., Maisaroh, S., Karya, A. & Husada, B. Hubungan Status Kesehatan Ibu Dengan Kejadian Preekamsi Di Rumah Sakit Tangerang. J. Ilmu Kesehat. Karya Bunda Husada 9, (2023).
Prasetya, P. Hubungan Anemia Trimester Pertama dengan Preeklampsia pada Ibu Hamil di Puskesmas Sidotopo Wetan Surabaya. (2018).
Tarisma, A. & Widyastuti, Y. Hubungan Anemia Ibu Hamil Trimester Tiga dengan Kejadian Preeklampsia Ibu Bersalin di RSUD Muntilan Kabupaten Magelang Tahun 2018. (2020).
Nanda, A. & Semarawisma, S. Association between anemia and preeclampsia: a case control study in Gorontalo region, Indonesia. J. Penelit. Int. di (2022).
Hamzah, S., Idris, I., Sanitaria, M. R.-G. & 2021, U. Antenatal care parameters that are the risk factors in the event of preeclampsia in primigravida. Elsevier.
Ridho, H. Hubungan Anemia Dengan Kejadian Preeklamsia Di Rumah Sakit Universitas Airlangga Surabaya Periode 1 Januari 2017 –31 Desember 2017. (2020).
Ameliai, E. & Sutarno, M. Influence Anemia Of The Event Preeclampsia In Maternal. Sains Kebidanan 10, 2721–9453 (2022).
Pujiyani, H. Faktor Risiko Kejadian Preeklampsia. J. Ilmu Kesehat. 12, 1410–234 (2018).
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva, Switz. World Heal. Organ. 1–6 (2011) doi:2011.
Agarwal, A. & Rets, A. Laboratory approach to investigation of anemia in pregnancy. J. Int. Lab. 43, 65–70 (2021).
Sircar, M., Thadhani, R. & Karumanchi, S. A. Pathogenesis of preeclampsia. Curr. Opin. Nephrol. Hypertens. 24, 131–138 (2015).
Sari, S. A., Fitri, N. L. & Dewi, N. R. Hubungan usia dengan kejadian anemia pada ibu hamil di Kota Metro. J. Wacana Kesehat. 6, (2021).
Wijayanti, E. & Qonitun, U. The Correlation Of Maternal Age And Gestational Age With Anemia In Pregnant Women At Puskesmas Meraurak, Tuban, East Java, Indonesia. J. Int. Penelit. Kebidanan, 2021, 1, (2021).
Triharini, M., Sulistyono, A., Adriani, M., Ners, S. D.-J. & 2019, U. The Effect of Health Promotion Model and Self Determination Theory Based Intervention on Anemia Prevention Behavior and Haemoglobin Level in Pregnant Women. Jurnal Ners, 14, 2502–5791 (2019).
Abu-Ouf, N. M. & Jan, M. M. The impact of maternal iron deficiency and iron deficiency anemia on child’s health. Saudi Med. J. 36, 146 (2015).
Nugraha, G. B. & Prasetyo, P. J. Anemia in Pregnancy as a Predisposing Factor of Severe Preeclampsia. J. Obstet. dan Ginekol. (2021).
Labir, I., Widarsa, I. & Suwiyoga, K. Anemia pada ibu hamil trimester pertama dan kedua meningkatkan risiko bayi berat lahir rendah di RS Wangaya , Denpasar. Public Heal. Prev. Med. Arch. 1, 19–23 (2013).
Rana, S., Lemoine, E., Granger, J. & Karumanchi, S. A. Preeclampsia: Pathophysiology, Challenges, and Perspectives. Circ. Res. 124, 1094–1112 (2019).
Perkumpulan Obstetri dan Ginekologi Indonesia. Pedoman Nasional Pelayanan Kedokteran Diagnosis dan Tata Laksana Pre-eklamsia. (2016).
Marniati, M., Rahmi, N., Healthcare, K. D.-J. O. & 2019, undefined. Analisis Hubungan Usia, Status Gravida dan Usia Kehamilan dengan Pre-Eklampsia pada Ibu Hamil di Rumah Sakit Umum dr. Zaionel Abidin Provinsi Aceh Tahun. Journal Healthcare Technology and Medicine. 2, 2615–109 (2016).
Hayashida, H., Nakamura, K., Ukon, K. & Sato, K. Atypical preeclampsia before 20 weeks of gestation with multicystic placenta, hyperreactio luteinalis, and elevated sFlt-1/PlGF ratio as manifestations of fetal triploidy: A case report. Case Reports Women’s Heal. 33, (2022).
Palupi, D. & Indawati, R. Faktor Risiko Kematian Ibu dengan Preeklampsia/Eklampsia dan Perdarahan di Provinsi Jawa Timur. J. Biometrika dan Kependud. (2014).
Karrar, S. & Hong, P. Preeclampsia. (2023).
RI, K. K. Pedoman Pelayanan Antenatal Terpadu. 3, (2020).
UK, N. G. A. Hypertension in Pregnancy: Diagnosis and Management (NG133). (2019).
Fox, R., Kitt, J., Leeson, P., Aye, C. Y. L. & Lewandowski, A. J. Preeclampsia: risk factors, diagnosis, management, and the cardiovascular impact on the offspring. J. Klin. (2019) doi:10.3390/jcm8101625.
ACOG. ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet. Gynecol. 133, e1–e25 (2019).
Ramakrishnan, V. & Poorana, D. Incidence of preeclampsia in antenatal anaemic mothers at the time of admission and maternal mortality in anaemia associated preeclampsia- a study at tertiary care referral centre. J. Evolusi Kedokt. dan (2017).
Haile, T. G. et al. Determinants of Preeclampsia among Women Attending Delivery Services in Public Hospitals of Central Tigray, Northern Ethiopia: A Case-Control Study. J. Pregnancy 2021, (2021).
Burwick, R., Newman, R., Amerika, M. R.-J. O. & & 2022, U. Mild Anemia and Risk of Postpartum Hemorrhage or Blood Transfusion in Preeclampsia.
Aznam, A. & Inayati, L. Relationship between age and parity of pregnant women anemia incidences in Mayangrejo. J. Biometrika dan Kependud. (2021).
Endeshaw, M., Abebe, F., Bedimo, M. & Asart, A. Diet and Pre-eclampsia: A Prospective Multicentre Case-Control Study in Ethiopia. Midwifery 31, 617–624 (2015).
Bilano, V. L., Ota, E., Ganchimeg, T., Mori, R. & Souza, J. P. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low- and middle-income countries: A WHO secondary analysis. PLoS One 9, (2014).
Copyright (c) 2024 Pirlina Umiastuti, Sri Umijati, Safira Raissa, Muhammad Fadhil, Khansa Raihani, Emyrazel Fahdizar, Neissya Nastiti, Mariska Nuriana, Siti Aria, Shabrina Nur Imanina

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.