Characteristics and Management of Laryngopharyngeal Reflux in The Elderly : A Case Report

Laryngopharyngeal reflux is a condition resulting from the retrograde flow of stomach acid through the distal esophagus into the laryngopharyngeal area. The prevalence of laryngo-pharyngeal reflux in the elderly population remains uncertain. Therefore, the symptoms, findings, and therapy for laryngopharyngeal reflux in the elderly require further investigation. To analyze the characteristics and management of laryngopharyngeal reflux in the elderly. A case of laryngopharyngeal reflux in a 70-year-old woman who frequently experiences sudden choking sensations is presented in this report. Other symptoms include hoarseness, a sensation of throat obstruction, and chest burning. We explored literature on laryngopharyngeal reflux in the elderly through PubMed, PMC, and Google Scholar databases to discuss the case. Laryngopharyngeal reflux in the elderly has a lower reflux symptoms index but a higher reflux finding score. Mental health factors significantly influence laryngopharyngeal reflux incidence in the elderly. Therefore, besides pharmaco-logical therapy, additional non-pharmacological therapies need to be considered to ensure effective laryngopharyngeal reflux treatment. Elderly patients diagnosed with laryngopharyngeal reflux have different presentations and management of the disease compared with younger patients.
INTRODUCTION
Laryngopharyngeal reflux (LPR) is a condition resulting from the retrograde flow of stomach acid through the distal esophagus into the laryngopharyngeal area. LPR induces laryngeal symptoms, including throat clearing, hoarseness, pain, throat irritation sensation, cough, excessive throat mucus, and dysphonia. The term LPR was first introduced in 1996 by Kauffman et al. Initially, LPR was considered another form of Gastroesophageal Reflux Disease (GERD) due to the reflux of gastric contents into the upper aerodigestive tract11. However, by 2002, the American Academy of Otolaryngology-Head and Neck Surgery defined LPR as the backflow of gastric contents into the laryngopharynx22. Specific GERD symptoms such as heartburn and regurgitation are not necessarily present in LPR patients, as LPR exhibits distinct clinical manifestations. In LPR, reflux of acid into the lower esophagus is considered normal and thus not diagnosed as GERD. LPR primarily emphasizes acid reflux into the upper esophagus, directly affecting the laryngopharynx11.
The progression of LPR is associated with high-fat diets, low-protein diets, stress or anxiety, and smoking. Meanwhile, obesity is reported to exa-cerbate the LPR. Due to its pathophy-siological, diagnostic, and therapeutic characteristics, LPR necessitates direct involvement from otolaryngology specialists22.
LPR in elderly patients and young patients is different, and this difference can be seen from the reflux score index (RSI), reflux finding score (RFS), and the therapy given.A study conducted by Lechien in 2021 stated that patients aged >60 years had lower RSI and higher RFS33. This is inversely proportional to young patients, namely higher RSI and lower RFS. On the other hand, the therapy given to elderly patients and young patients is also different. This is because in elderly patients it is necessary to consider that mental health in the form of somatic anxiety can influence the incidence of LPR, so that in addition to pharmacological therapy giving PPI to LPR it is necessary to give additional medication such as anti-anxiety drugs and non-pharmacological therapy such as anti-reflux diet, healthy lifestyle, and cognitive behavioral therapy(CBT) specifically for elderly patients with symptoms of anxiety/depression so that LPR treatment can be effective4–6456.
CASE REPORT
A 70-year-old woman presented with complaints of frequent sudden choking sensations and difficulty breathing for the past 3 months. Over the last 3 months, the patient reported experiencing >5 attacks. Additionally, the patient mentioned frequent throat clearing but difficulty in expectorating phlegm and occasional dry cough, albeit denying any changes in voice/ hoarseness. Over the past year, the patient has often experienced heartburn and reported sleeping disturbances for the past three months. There were no complaints regarding the ears and nose. Reflux symptom index (RSI) queried during the anamnesis revealed breathing difficulty (4), frequent throat clearing (2), heartburn, warmth sensation, digestive disturbances (3), and coughing (2), resulting in a score of 111.
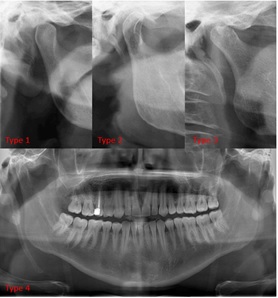
Upon physical examination, the patient was in good overall condition with mild pain, alert mentation, blood pressure of 160/90 mmHg, heart rate of 89 beats per minute, respiratory rate of 20 breaths per minute, and temperature of 36.8°C. General status was within normal limits. Local examination revealed granulation in the oropharynx and post-nasal drip. Ancillary examination was conducted using fiber optic laryngoscopy (FOL), as shown in Figure 1.
Figure 1.FOL examination results
The FOL examination results were adjusted with the reflux finding score (RFS) to aid in the diagnosis of LPR. The identified RFS included subglottic edema (2), arytenoid hyperemia (2), severe diffuse laryngeal edema (3), severe posterior commissure hypertrophy (3), and endolaryngeal mucus (2), resulting in a score of 12.
Based on the history, physical examination, and ancillary tests, the patient was diagnosed with LPR. Medication therapy for the patient consisted of Omeprazole tablets 40 mg twice daily, Sucralfate syrup 3 times daily, and Chlordiazepoxide HCL-Clidinium bromide tablets 3 times daily as an anxiolytic. Non-medication treatment included controlling dietary patterns (reducing intake of fatty and acidic foods) and setting a priority scale of daily activities.
DISCUSSION
LPR represents an inflammatory process in the upper respiratory tract, particularly in the larynx, involving the reflux of gastroduodenal fluids onto the laryngeal mucosa, resulting in morphological changes in the aerodigestive tract. Gastroduodenal fluids containing pepsin, trypsin, bile salts, and other proteins can irritate the lower esophagus, stimulating chemoreceptors and triggering cough reflexes, leading to mucosal injury, inflammatory reactions, epithelial thickening, and microtrauma4,747.
In the elderly, the mechanisms underlying LPR involve reduced salivary flow and bicarbonate secretion, which are associated with decreased acid neutralization during reflux. Additionally, in the elderly, esophageal motility and pressures of the Lower Esophageal Sphincter (LES) and Upper Esophageal Sphincter (UES) weaken, theoretically contributing to increased LPR incidence. The diagnosis of LPR is established based on the Reflux Symptom Index (RSI), Reflux Finding Score (RFS), positive response to empirical therapy trials, or Hypopharyngeal–Esophageal Multichannel Intraluminal Impedance pH monitoring (HEMII-pH). However, diagnosis confirmation of LPR is more commonly achieved using RSI and RFS7,878.
RSI items are essential questions that need to be asked when patients present with voice changes or hoarseness in otolaryngology clinics. Sataloff RT mentioned in 2010 that 10% of patients visiting ENT clinics have LPR, with almost 100% complaining of hoarseness upon presentation99. According to a systematic review by Lechien JR in 2022, the most common clinical symptoms of LPR patients include dysphonia, throat irritation sensation, throat pain, odynophagia, throat
Widiantari IAA, Sucipta IW. Karakteristik penderita laryngopharyngeal reflux yang didiagnosis berdasarkan reflux symptom index dan reflux finding score di Poliklinik THT-KL RSUP Sanglah Tahun 2015-2017. Medicina (B Aires). 2019;50(3):457-461. doi:10.15562/medicina.v50i3.678
Lechien JR, Saussez S, Muls V, et al. Laryngopharyngeal reflux: A state-of-the-art algorithm management for primary care physicians. J Clin Med. 2020;9(11):1-18. doi:10.3390/jcm9113618
Lechien JR, Mouawad F, Bobin F, Bartaire E, Crevier-Buchman L, Saussez S. Review of management of laryngopharyngeal reflux disease. Eur Ann Otorhinolaryngol Head Neck Dis. 2021;138(4):257-267. doi: 10.1016/j.anorl.2020.11.002
Lechien JR, Carroll TL, Bobin F, et al. Influence of Age and Sex on Clinical and Therapeutic Features of Laryngopharyngeal Reflux. Otolaryngol - Head Neck Surg (United States). 2022;166(3):468-476. doi:10.1177/01945998211020284
Krause AJ, Walsh EH, Weissbrod PA, Taft TH, Yadlapati R. An update on current treatment strategies for laryngopharyngeal reflux symptoms. Ann N Y Acad Sci. 2022;1510(1):5-17. doi:10.1111/nyas.14728
Lechien JR, Finck C, Huet K, et al. Impact of age on laryngopharyngeal reflux disease presentation: a multi-center prospective study. Eur Arch Oto-Rhino-Laryngology. 2017;274(10):3687-3696. doi:10.1007/s00405-017-4671-z
Lechien JR. Treating and Managing Laryngopharyngeal Reflux Disease in the Over 65s: Evidence to Date. Clin Interv Aging. 2022;17(November):1625-1633. doi:10.2147/CIA.S371992
Kuo CL. Laryngopharyngeal Reflux: An Update. Arch Otorhinolaryngol Neck Surg. 2019;3(1):1-7. doi:10.24983/scitemed.aohns.2019.00094
Mishra P, Agrawal D, Chauhan K, Kaushik M. Prevalence of Laryngopharyngeal Reflux Disease in Indian Population. Indian J Otolaryngol Head Neck Surg. 2022;74(s2):1877-1881. DOI: 10.1007/s12070-020-01882-1
Aulia W. Refluks Laringofaring. Scr SCORE Sci Med J. 2020;2(1):64-67. doi:10.32734/scripta.v2i1.3956
Vance D, Alnouri G, Shah P, et al. The Validity and Reliability of the Reflux Finding Score. J Voice. 2023;37(1):92-96. doi:10.1016/j.jvoice.2020.11.008
Cervera-Paz FJ, Jordano-Cabrera M. Characterisation of laryngo-pharyngeal reflux disease in old and ageing patients. Acta Otorrinolaringol Esp. 2019;70(3):151-157. doi:10.1016/j.otorri.2018.05.002
Massawe WA, Nkya A, Abraham ZS, et al. Laryngopharyngeal reflux disease, prevalence and clinical characteristics in ENT department of a tertiary hospital Tanzania. World J Otorhinolaryngol - Head Neck Surg. 2021;7(1):28-33. DOI: 10.1016/j.wjorl.2020.04.009
Kang JW, Lee MK, Lee YC, Ko S gyu, Eun YG. Somatic anxiety in patients with laryngopharyngeal reflux. Laryngoscope Investig Otolaryngol. 2023;8(5):1288-1293. doi:10.1002/lio2.1138
Muna Z, Adyani L. Analisis Kesehatan Mental Pada Lansia (Memahami Kebersyukuran Pada Lansia Muslim di Aceh Utara). J Psikol Terap. 2021;3(1):7. doi:10.29103/jpt.v3i1.3636
Grover S, Sahoo S, Chakrabarti S, Avasthi A. Anxiety and somatic symptoms among elderly patients with depression. Asian J Psychiatr. 2019;41(July 2018):66-72. doi:10.1016/j.ajp.2018.07.009
Rompas KI, Mengko SK, Palandeng OELI. Pendekatan Diagnostik Refluks Laring Faring. e-CliniC. 2021;9(2):457. doi:10.35790/ecl.v9i2.34596
Lin Y, Peng S. Current Treatment of Laryngopharyngeal Reflux. Ear, Nose Throat J. 2023;(37). doi:10.1177/01455613231180031
Curtiss JE, Levine DS, Ander I, Baker AW. Cognitive-Behavioral Treatments for Anxiety and Stress-Related Disorders. Focus (Madison). 2021;19(2):184-189. doi:10.1176/appi.focus.20200045
Bogucki OE, Craner JR, Berg SL, et al. Cognitive Behavioral Therapy for Anxiety Disorders: Outcomes From a Multi-State, Multi-Site Primary Care Practice. J Anxiety Disord. 2021;78(September 2020):102345. doi:10.1016/j.janxdis.2020.102345
Cui N, Dai T, Liu Y, et al. Laryngopharyngeal reflux disease: Updated examination of mechanisms, pathophysiology, treatment, and association with gastroesophageal reflux disease. World J Gastroenterol. 2024;30(16):2209-2219. DOI: 10.3748/wjg.v30.i16.2209
Kenny C. Spotlight on: Nature, assessment, and management of laryngopharyngeal reflux. Adv Commun Swallowing. 2023;26(2):89-97. doi:10.3233/acs-230011
Copyright (c) 2024 Wahyu Ikhsan, Aliyah Hidayati

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.