The Influence of Family-Expressed Emotion on the Risk of Relapse in Patients with Schizophrenia: Outcomes from a Community Medicine Intervention
Schizophrenia is a syndrome characterized by fundamental deviations in thinking, perception, and affect. Expressed emotion (EE) is a crucial risk factor in influencing the occurrence of relapse. In Indonesia, there is still no community therapy activity related to the family EE against the risk of relapse of schizophrenia patients. This is the underlying need for community psychiatry activities against families of patients with schizophrenia and related parties. This cross-sectional study was conducted in Puri, Mojokerto, Indonesia. The method was divided into three stages: field introduction, community diagnosis, and community therapy. In 36 schizophrenia patients, it was found that the level of EE experienced by the patients was relatively low, and the risk of recurrence within one year was around 43.27%. Based on these findings, the families of schizophrenia patients in Puri District can express good positive emotions towards their patients, which is in line with the relatively low risk of relapse. The author did an EE assessment by sharing a questionnaire as a short-term evaluation of the occurrence of relapse.As a continuation of the program, long-term evaluation will be returned to the community health centre and carried out by the program holder. Community medicine benefits community health centers, communities, and students by increasing family and community awareness of schizophrenia and improving the quality of community health centers and public health. Students also learn how to educate families with schizophrenia.
INTRODUCTION
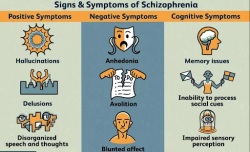
Schizophrenia is a chronic mental disorder characterized by cognitive impairment, delusions, hallucinations, abnormal thoughts, and irregular behavior. There are 24 million people worldwide suffering from Schizophrenia. Most symptoms of schizophrenia appear in their 20s and older adults, and are more common in men11. Each region in Indonesia has different rates of schizophrenia incidence, one of which is in the Puri, Mojokerto, where 96 patients were diagnosed with Schizophrenia. Schizophrenic patients undoubtedly experience disability, which is often caused by negative symptoms (loss or deficit), cognitive impairment (disturbance in attention, memory), positive symptoms (suspicion, delusions, and hallucinations), and executive function disorders22.
A total of 81.9% of schizophrenic patients experience relapses within five years after the first episode appears. Relapses are the return or worsening of the disease after the remission period33. There are several risk factors for schizophrenia relapses, including drug-taking compliance, interpersonal relationships, daily living ability, family communication, participation in therapy rehabilitation, and history of hospital admission in the past year. Among the factors that affect relapses, relationships with families become one of the crucial factors in determining prognosis compared to other factors44.
Expressed Emotion (EE) is interpreted as emotions expressed in the family environment between caregivers and schizophrenic patients and other psychiatric disorders. it has been found that EE can be used in predicting relapse symptoms or relapse in various mental disorders55. EE has five components: critical comments (CC), hostility, emotional over-involvement (EOI), positive remarks, and warmth. CCs are influenced by negative evaluation and tone of voice when conveying their feelings (anger, rejection, irritability, ignorance, blame, negligence, etc.). EOI includes the feelings or actions of overprotecting and self-sacrificing from the family to the patient66. In Indonesia, there is still no community therapy activity related to the family EE against the risk of relapse of schizophrenia patients. This is the underlying need for community psychiatry activities against families of patients with schizophrenia and related parties.
Community Medicine activities held by the Faculty of Medicine, Universitas Airlangga, consist of three activities. The first is WWF (Work With Family), which aims to improve students’ ability to enhance their individual and family health care. Each student in a team gets a specific case and then performs a comprehensive examination, home visits, and solutions related to the problem.
The second is WWHT (Work With Health Teams). The students are trained to perform holistic health care management in primary health care. The third is WWC (Work With Community), where this activity aims to improve health in the scope of the community. WWC is done through 3 stages: field recognition, community diagnosis, and community therapy.
MATERIALS AND METHODS
The method can be divided into three stages: field recognition, community diagnosis, and community therapy, which are completed within three weeks.
1. Community anamnesis in the form of field recognition
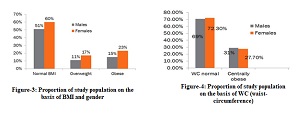
Researchers conducted interviews with the Puri Community Health Center to get a general picture of the problems in the Puri Community Health Center's working area. After learning about the high number of schizophrenia cases, researchers conducted a direct survey with the families of schizophrenia patients to assess the emotions expressed by the family towards the patient using the Family Questionnaire (FQ) questionnaire and the risk of recurrence for schizophrenia patients using the SMART Card. The FQ is a questionnaire that describes emotions and emotional behavior, or expressed emotion, that consists of 20 questions with the answer options never, rarely, often, and very often. The SMART card is a measuring tool resulting from research on The Biopsychocultural-spiritual factors influencing relapse of schizophrenic patients by Margarita M. Maramis, M. Sofyan Almahdy, and Atika77. This card contains 12 questions that help predict the risk, in percentage terms, of the likelihood of recurrence of adult schizophrenia within 1 year. Samples were taken by purposive sampling. The data obtained were analyzed univariately using SPSS-27.
2. Community Diagnosis
The workshop was held at the Mlaten, Puri, Mojokerto, Indonesia. Representatives from the Puri Community Health Center, Mental health cadres for villages spread across Puri District, village officials, psychiatry residents, and representatives from the patient's family attended. The results of the survey obtained at the field recognition stage were presented by representatives of young doctors, focusing on problems related to the expression of family emotions towards patients and the risk of recurrence of schizophrenia patients in Puri, Mojokerto, Indonesia.
Cross-sector participants were divided into five groups to discuss risk factors and solutions to community problems. The discussion session ended with each participant filling in suggested solutions for the two things that had been discussed previously. The proposed suggestions were presented, and solutions were determined using the Nominal Group Technique (NGT) Delbecq method, followed by all cross-sector participants present. NGT is a structured group-based technique used to create an agreement. Participants were asked to answer questions individually based on predetermined, structured questions written by the facilitator. Next, participants were asked to prioritize ideas and suggestions issued by group members collectively88. There is one solution that is possible and agreed upon. This was followed by an oral and written Memorandum of Understanding (MoU) in the form of a commitment to consider the survey results that had been carried out through distributing questionnaire research instruments. The MoU results in a joint commitment to carry out community therapy to solve this problem. Community diagnosis is carried
World Health Organization. Schizophrenia. World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia
Srisudha B, Kattula D, Devika S, Rachana A. 2022. Cognitive dysfunction and disability in people living with schizophrenia. Journal of Family Medicine and Primary Care, 11(6):2356. DOI: 10.4103/jfmpc.jfmpc_396_21
Iliades, Schizophrenia Relapse: What to Know. 2014.. Available from: https://www.everydayhealth.com/hs/schizophrenia-caregiver-guide/recognizing-and-preventing-relapse/.
Mi W-F, Chen X-, Fan T-T, Tabarak S, Xiao J-B, et al. 2020. Identifying modifiable risk factors for relapse in patients with schizophrenia in China. DOI: 10.3389/fpsyt.2020.574763
Yimam, B, Soboka, M, Getachew, Y et al. 2022. Expressed emotion of caregivers among schizophrenic patients visiting Jimma University Medical Center Psychiatry Outpatient Unit, Southwest Ethiopia. Ann Gen Psychiatry, 21(27). DOI: 10.1186/s12991-022-00404-3
Zanetti ACG, Vedana KGG, Pereira CCM, et al. 2019. Expressed emotion and socio-demographic and clinical factors in families of Brazilian patients with schizophrenia. International Journal of Social Psychiatry, 65(1):56-63. DOI: 10.1177/0020764018815207
Maramis MM, Almahdy MS, Atika. 2020. ‘SMART’ Card to Predict Recurrence in Schizophrenic Patients. Airlangga University. DOI: 10.1177/00207640211065678
Hugé, J., & Mukherjee, N. (2018). The nominal group technique in Ecology & Conservation: Application and challenges. Methods in Ecology and Evolution, 9(1), 33–41. DOI: 10.1111/2041-210x.12831
Do TTH, Bui QTT, Ha BTT, Le TM, Le VT, Nguyen QT, Lakin KJ, Dang TT, Bui LV, Le TC, Tran ATH, Pham HTT, Nguyen TV. 2023. Using the WHO Self-Reporting Questionnaire-20 (SRQ-20) to Detect Symptoms of Common Mental Disorders among Pregnant Women in Vietnam: a Validation Study. Int J Womens Health, Apr 14;15:599-609. DOI: 10.2147/IJWH.S404993
Ma C F, Chan SKW, Chung YL, Ng SM, Hui CLM, Suen YN, & Chen EYH. 2021. The predictive power of expressed emotion and its components in relapse of schizophrenia: a meta-analysis and meta-regression. Psychological Medicine, 51(3), 365–375. DOI: 10.1017/S0033291721000209
Bailey RC, Grenyer BFS. 2014. The relationship between expressed emotion and well-being for families and carers of a relative with borderline personality disorder. Personality and Mental Health, Sept 4;9(1):21–32. DOI: 10.1002/pmh.1273
Ghosh R & Ahmed N. 2019. A study to Assess the Relationship between Stigma and Expressed Emotion Among the Primary Caregivers of Persons with Schizophrenia Attending Outpatient Department of Lokopriyo Gopinath Bordoloi Regional Institute of Mental Health Tezpur. Indian Journal of Psychiatric Nursing, 1(16), 2-6. DOI: 10.4103/IOPN.IOPN_5_19
Sariah AE, Outwater AH, Malima KI. 2014. Risk and protective factors for relapse among individuals with schizophrenia: A qualitative study in Dar es Salaam, Tanzania. BMC Psychiatry, Aug 30;14(1). DOI: 10.1186/s12888-014-0240-9
Shamsaei F, Cheraghi F, Bashirian S. 2015. Burden on Family Caregivers Caring for Patients with Schizophrenia. Iran J Psychiatry, Sep;10(4):239-45 https://ijps.tums.ac.ir/index.php/ijps/article/view/576
Caqueo-Urízar A, Rus-Calafell M, Urzúa A, Escudero J, Gutiérrez-Maldonado J. 2015. The role of family therapy in the management of schizophrenia: challenges and solutions. Neuropsychiatr Dis Treat, Jan 14;11:145-51. DOI: 10.2147/NDT.S51331
Guendelman S., Medeiros S., Rampes H. (2017). Mindfulness and Emotion Regulation : Insights from Neurobiological, Psychological and Clinical Studies. National Library of Medicine. Front Psychol.1. DOI: 10.3389/fpsyg.2017.00220
Zhang ZJ, Lo HH, Ng SM, Mak WW, Wong SY, Hung KS, et al. 2023. The effects of a mindfulness-based family psychoeducation intervention for the caregivers of young adults with first-episode psychosis: A randomized controlled trial. International Journal of Environmental Research and Public Health, Jan 5;20(2):1018. DOI: 10.3390/ijerph20021018
Andayani B., Ancok D., Wulan R. 2018. From Love to Family Happiness: a Theoretical Model for Javanese Family. European Journal of Social Sciecne Education and Research, Sciendo; 5( 1), 25-35. DOI: 10.2478/ejser-2018-0003
Yu L. 2022. Analysis of “harmony” and “Unity” concepts in Indonesian and Chinese culture. MANDARINABLE : Journal of Chinese Studies, Aug 12;1(1):10–6. DOI:10.20961/mandarinable.v1i1.326
Subandi MA, Praptomojati A, Marchira CR, DelVecchio Good M-J, Good BJ. 2020. Cultural explanations of psychotic illness and care-seeking of family caregivers in Java, Indonesia. Transcultural Psychiatry, Apr 14;58(1):3–13. DOI: 10.1177/1363461520916290
Millier A, Schmidt U, Angermeyer MC, Chauhan D, Murthy V, Toumi M, et al. 2014. Humanistic burden in schizophrenia: A literature review. J Psychiatr Res, 54, 85–93. DOI: 10.1016/j.jpsychires.2014.03.021
Tamizi Z, Fallahi-Khoshknab M, Dalvandi A, Bakhshi E, Mohammadi E, Mohammadi-Shahboulaghi F. 2020. Caregiving burden in family caregivers of patients with schizophrenia: A qualitative study. Journal of Education and Health Promotion, Jan;9(12). DOI: 10.4103/jehp.jehp_356_19
Lee Y. Bierman A., Penning M. dan Kemp C. (2020). Psychological well-being among informal caregivers in the Canadian longitudinal study on aging: why the location of care matters. The Journals of Gerontology: Series B, 75(10), 2207–2218. DOI: 10.1093/geronb/gbaa159
Copyright (c) 2025 Muhammad Bagus Wira, Sarah Nia, Ramidha Syaharani, Ezrin Syariman, Karindra Amadea, Anastasia Pearl, Khansa Talitha, Margarita Maria Maramis

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.