Diet and Non-Alcoholic Fatty Liver Disease (NAFLD): Advances and Management Strtegies : A Comprehensive Review

Global public health is at risk from non-alcoholic fatty liver disease, or NAFLD. Fat accumulation in the liver is associated with chronic liver disease (NAFLD), even in the absence of significant alcohol consumption. It could have anything to do with liver inflammation and fibrosis. Because non-communicable diseases have become more common over the past few years, changing one’s lifestyle has drastically altered the priorities for health.Between 1990 and 2017, the number of people worldwide with NAFLD grew from 19.34 million to 29.49 million. An estimated 35.4% of Indians are believed to have NAFLD. Nonalcoholic fatty liver disease is the term used when there is no alcohol intake, and ectopic fat deposition exceeds 5% of the weight of the liver (NAFLD). It encompasses a broad range of morphologically diverse liver abnormalities, from basic steatosis to severe forms like non-alcoholic steatohepatitis (NASH), a progressive form of the disease marked by fibrosis, hepatocyte ballooning degeneration, and lobule inflammation. Obesity, diabetes, dyslipidemia, and the so-called insulin resistance or metabolic syndrome are linked to primary NAFLD/NASH. Rarely, secondary NAFLD/NASH can be linked to a variety of illnesses, including pancreatic duodenal resection, endocrine disorders, polycystic ovary syndrome, and sleep apnea. Today's kids face an unparalleled dietary challenge. Food is abundant, yet a growing proportion of kids are overweight or obese due to inadequate nutrition. Hyperinsulinemia with insulin resistance seems to be crucial in pediatric NAFLD. Understanding pediatric NAFLD's pathophysiology is anticipated to enhance our understanding of the condition. Additionally, finding prevention treatments for pediatric NAFLD is imperative for the well-being of children.
INTRODUCTION
At least one-third of the general population across all age groups is afflicted with Non-Alcoholic Fatty Liver Disease (NAFLD), also known as Metabolic Dysfunction Associated Liver Disease (MASLD), one of the primary causes of chronic liver problems globally. The term NAFLD refers to a group of liver conditions that include cirrhosis, non-alcoholic steatohepatitis (NASH), and simple steatosis, which is defined as macrovesicular steatosis in hepatocytes without inflammation11.
Globally, the most frequent cause of chronic liver disease is NAFLD. This disease is categorized as the hepatic manifestation of the Metabolic Syndrome due to its strong correlation with obesity, insulin resistance (IR), and dyslipidaemia. In the absence of alcohol usage, ectopic fat accumulation larger than 5% of the liver weight is predictive of NAFLD. In the last ten years, obesity and insulin resistance have emerged as the two primary risk factors for NAFLD. Even in individuals with comparable body mass indices (BMIs), NAFLD can present with a broad spectrum of clinical symptoms. Currently, liver biopsy is the most reliable method of diagnosing NAFLD.
There is not a single therapy strategy that is acceptable to everyone when treating illness. However, a mix of dynamic clinical characteristics impacted by pharmacological therapies and lifestyle choices may help identify valid score-based methods for predicting liver damage and customizing treatment options22. Although NAFLD is commonly linked to obesity, metabolic problems can also be the cause of it in non-obese persons. People with the advancing form of the disease and associated fibrosis, in addition to having NASH, are often more likely to have components of the metabolic syndrome, notably type 2 diabetes and visceral obesity. Patients with NAFLD who have multiple metabolic syndrome components are at a higher risk of dying33.
NASH was discovered initially in adults in the late 1970s, and in children in the early 1980s. It was not until 25 years later that NAFLD’s high prevalence in adults, kids, and teenagers was recognized. As the proportion of children who are obese rises, NAFLD is becoming the most common chronic liver condition affecting children. The dietary challenges that today’s youth face are unsurpassed. Food is plentiful, but non-communicable diseases are becoming more common11.
Since obesity and metabolic disorders are frequently associated with NAFLD, it is thought that NAFLD represents the adult metabolic syndrome’s hepatic manifestation. NAFLD has been seen in adults who are slender and underweight, although the condition was formerly thought to be the result of obesity. Since the conclusion of the previous decade, there has been an upsurge in the number of subjects categorized as lean and non-obese NAFLD. There is proof that malnutrition can result in metabolic issues and eventually lead to NAFLD. Due to truncal fat accumulation, altered metabolism, and a loss of muscle mass, thin and underweight adults may also develop NAFLD. Even if an adult is not obese or overweight, their food intake, particularly a diet heavy in fat and sugar, can still have an impact on their chance of developing NAFLD.
It was discovered that patients with lean NAFLD had more pronounced metabolic disturbances. Reduced muscle mass, altered body composition, and reduced lipid turnover may all contribute to metabolic abnormalities in lean individuals. Dietary consumption, particularly a high-fructose, high-fat diet, may potentially contribute to the onset of non-alcoholic fatty liver disease, or NAFLD, in individuals who are not obese or overweight. NAFLD in underweight and thin individuals can also be attributed to genetic predispositions, type 2 diabetes mellitus, and other disorders associated with the metabolic syndrome. According to multicentre cohort research, those with NAFLD who are underweight or thin may also be more likely to die than those who are overweight or obese. Studies show that 5-8% of people with a BMI ≤ 25 kg/m2 may have NAFLD. Furthermore, it has been discovered that 8–19% of Asians with an average body mass index ≤ 25 kg/m2 have NAFLD44.
OVERVIEW
Prevalence
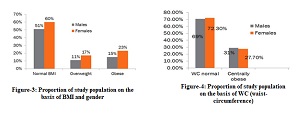
One of the leading causes of chronic liver disorders in the world is NAFLD, commonly referred to as MASLD. According to estimates, 32% of people globally have NAFLD; men are more likely to have it (40%) than women (26%). Due to global differences in obesity rates, genetic, and socioeconomic factors, NAFLD incidence varies significantly by geography55.
According to a children's autopsy study that employed liver histology to gauge the prevalence of non-alcoholic fatty liver disease (NAFLD) in the US, 9.6% of children between the ages of 2 and 19 had the condition. Fatty liver became more common as people grew older; at its highest, it was 17.3% among those in the 15- to 19-year-old range and 0.7% for people in the 2-4 age range66. NAFLD is now the second-leading cause of liver transplantation in the United States as a result of its increasing occurrence33. The prevalence of fatty liver rose with age, peaking at 17.3% for those between the ages of 15 and 19 and 0.7% for those between the ages of 2-466.
According to data from the World Health Organization, the number of overweight and obese individuals worldwide has surpassed that of underweight and malnourished individuals. A study done in the UK claims that in the last 40 years, the prevalence of obesity among kids and young adults (between the ages of 5 and 19) has risen tenfold77
Roberts EA. Pediatric nonalcoholic fatty liver disease (NAFLD): a “growing” problem?. Journal of hepatology. 2007 Jun 1;46(6):1133-42. DOI: 10.1016/j.jhep.2007.03.003
Meroni M, Longo M, Tria G, Dongiovanni P. Genetics is of the essence to face NAFLD. Biomedicines. 2021 Sep 30;9(10):1359. DOI: 10.3390/biomedicines9101359
Arshad T, Paik JM, Biswas R, Alqahtani SA, Henry L, Younossi ZM. Nonalcoholic Fatty Liver Disease Prevalence Trends Among Adolescents and Young Adults in the U nited S tates, 2007‐2016. Hepatology Communications. 2021 Oct;5(10):1676-88. DOI: 10.1002/hep4.1760
Fahim SM, Chowdhury MA, Alam S. Non-alcoholic fatty liver disease (NAFLD) among underweight adults. Clinical nutrition ESPEN. 2020 Aug 1;38:80-5. DOI: 10.1016/j.clnesp.2020.06.002
Teng ML, Ng CH, Huang DQ, Chan KE, Tan DJ, Lim WH, Yang JD, Tan E, Muthiah MD. Global incidence and prevalence of nonalcoholic fatty liver disease. Clinical and molecular hepatology. 2022 Dec 14;29(Suppl):S32. DOI: 10.3350/cmh.2022.0365
Barshop NJ, Sirlin CB, Schwimmer JB, Lavine JE. epidemiology, pathogenesis and potential treatments of paediatric non‐alcoholic fatty liver disease. Alimentary pharmacology & therapeutics. 2008 Jul;28(1):13-24. DOI: 10.1111/j.1365-2036.2008.03703.x
Paik JM, Mir S, Alqahtani SA, Younossi Y, Ong JP, Younossi ZM. Dietary risks for liver mortality in NAFLD: global burden of disease data. Hepatology Communications. 2022 Jan;6(1):90-100. DOI: 10.1002/hep4.1707
Jasirwan CO, Lesmana CR, Hasan I, Sulaiman AS, Gani RA. The role of gut microbiota in non-alcoholic fatty liver disease: pathways of mechanisms. Bioscience of microbiota, food and health. 2019;38(3):81-8. DOI: 10.12938/bmfh.18-032
Jain V, Jana M, Upadhyay B, Ahmad N, Jain O, Upadhyay AD, Ramakrishnan L, Vikram NK. Prevalence, clinical & biochemical correlates of non-alcoholic fatty liver disease in overweight adolescents. Indian Journal of Medical Research. 2018 Sep 1;148(3):291-301. DOI: 10.4103/ijmr.IJMR_1966_16
Temple JL, Cordero P, Li J, Nguyen V, Oben JA. A guide to non-alcoholic fatty liver disease in childhood and adolescence. International journal of molecular sciences. 2016 Jun 15;17(6):947. DOI: 10.3390/ijms17060947
Paschos P, Paletas K. Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009 Jan;13(1):9. https://www.hippokratia.gr/2018/09/14/non-alcoholic-fatty-liver-disease-and-metabolic-syndrome/
Fang YL, Chen H, Wang CL, Liang L. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: From “two hit theory” to “multiple hit model”. World journal of gastroenterology. 2018 Jul 7;24(27):2974. DOI: 10.3748/wjg.v24.i27.2974
Hegarty R, Deheragoda M, Fitzpatrick E, Dhawan A. Paediatric fatty liver disease (PeFLD): all is not NAFLD–pathophysiological insights and approach to management. Journal of hepatology. 2018 Jun 1;68(6):1286-99. DOI: 10.1016/j.jhep.2018.02.006
Marušić M, Paić M, Knobloch M, Liberati Pršo AM. NAFLD, insulin resistance, and diabetes mellitus type 2. Canadian Journal of Gastroenterology and Hepatology. 2021;2021(1):6613827. DOI: 10.1155/2021/6613827
Wong VW, Zelber‐Sagi S, Cusi K, Carrieri P, Wright E, Crespo J, Lazarus JV. Management of NAFLD in primary care settings. Liver International. 2022 Nov;42(11):2377-89. DOI: 10.1111/liv.15404
Piazzolla VA, Mangia A. Noninvasive Diagnosis of NAFLD and NASH. Cells. 2020 Apr 17;9(4):1005. DOI: 10.3390/cells9041005
Fujii H, Kawada N, Japan Study Group of Nafld (JSG-NAFLD). The role of insulin resistance and diabetes in nonalcoholic fatty liver disease. International journal of molecular sciences. 2020 May 29;21(11):3863. DOI: 10.3390/ijms21113863
Noureddin M, Zelber‐Sagi S, Wilkens LR, Porcel J, Boushey CJ, Le Marchand L, Rosen HR, Setiawan VW. Diet associations with nonalcoholic fatty liver disease in an ethnically diverse population: the multiethnic cohort. Hepatology. 2020 Jun;71(6):1940-52. DOI: 10.1002/hep.30967
Liu X, Peng Y, Chen S, Sun Q. An observational study on the association between major dietary patterns and non-alcoholic fatty liver disease in Chinese adolescents. Medicine. 2018 Apr 1;97(17):e0576. DOI: 10.1097/MD.0000000000010576
Mirmiran P, Amirhamidi Z, Ejtahed HS, Bahadoran Z, Azizi F. Relationship between diet and non-alcoholic fatty liver disease: a review article. Iranian journal of public health.2017Aug;46(8):1007. https://ijph.tums.ac.ir/index.php/ijph/article/view/10599/5246
Yasutake K, Kohjima M, Kotoh K, Nakashima M, Nakamuta M, Enjoji M. Dietary habits and behaviors associated with nonalcoholic fatty liver disease. World Journal of Gastroenterology: WJG. 2014 Feb 2;20(7):1756. DOI: 10.3748/wjg.v20.i7.1756
Alwahsh SM, Gebhardt R. Dietary fructose as a risk factor for non-alcoholic fatty liver disease (NAFLD). Archives of toxicology. 2017 Apr;91:1545-63. DOI: 10.1007/s00204-016-1892-7
Asbaghi O, Emamat H, Kelishadi MR, Hekmatdoost A. The association between nuts intake and non-alcoholic fatty liver disease (NAFLD) risk: a case-control study. Clinical nutrition research. 2020 Jul;9(3):195. DOI: 10.7762/cnr.2020.9.3.195
Cardoso BR, Tan SY, Daly RM, Dalla Via J, Georgousopoulou EN, George ES. Intake of nuts and seeds is associated with a lower prevalence of nonalcoholic fatty liver disease in US adults: findings from 2005–2018 NHANES. The Journal of Nutrition. 2021 Nov 1;151(11):3507-15. DOI: 10.1093/jn/nxab253
Munteanu MA, Nagy GA, Mircea PA. Current management of NAFLD. Clujul medical. 2016;89(1):19. DOI: 10.15386/cjmed-539
Cardoso AC, de Figueiredo‐Mendes C, A. Villela‐Nogueira C. Current management of NAFLD/NASH. Liver International. 2021 Jun;41:89-94. DOI: 10.1111/liv.14869
Copyright (c) 2025 Syeda Farha S, Sheetal R

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.