Impact of the Elimination of the National Health Insurance (BPJS Health) Service Classes on Access and Quality of Healthcare in Indoneseia: A Systematic Review
Downloads
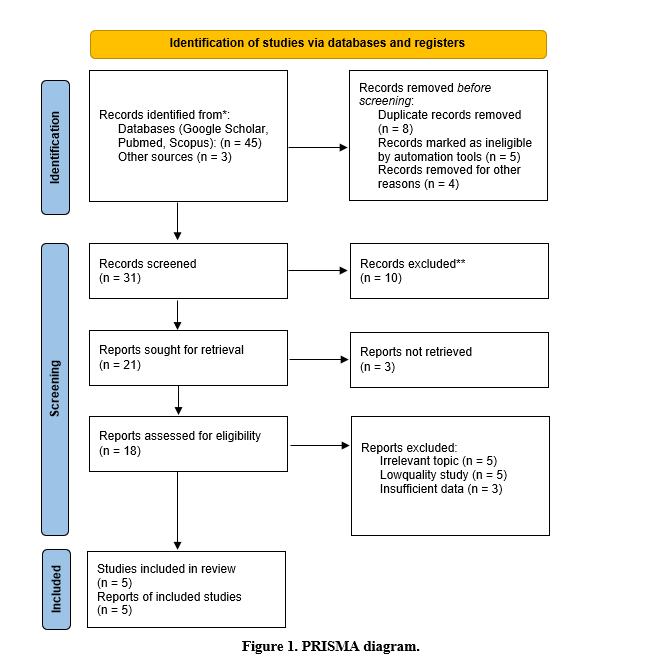
This study aims to analyze the impact of eliminating BPJS Health classes and implementing the Standard Inpatient Class (KRIS) in Indonesia, focusing on healthcare access, service quality, financial sustainability, and governance. The policy was introduced to promote social equity and reduce disparities in healthcare delivery. A systematic literature review was conducted using databases such as Google Scholar, PubMed, and Scopus, covering studies published between 2019 and 2024. The selected literature met inclusion and exclusion criteria to ensure relevance and quality, and a narrative synthesis was applied to identify major patterns and policy implications.The findings indicate that KRIS can improve fairness in healthcare access and simplify administrative processes. However, significant challenges remain, especially regarding hospital preparedness in less developed regions, where overcrowding, longer waiting times, and potential declines in service quality are likely to occur. The transition from a classbased system to a standardized model also raises financial concerns, particularly about sustainability and equity in funding. In addition, governance weaknesses and limited policy communication have led to uncertainty and public hesitation.Overall, KRIS reflects a progressive step toward healthcare equity but demands careful implementation. Sustainable financing, improved hospital capacity, effective governance, and active public participation are essential for ensuring its success. Future studies should continue exploring financial mechanisms and regional readiness to guide more inclusive and sustainable policy development.
Pramana C, Priastuty W. Perspektif Masyarakat Pengguna BPJS Kesehatan mengenai Kebijakan Kelas Rawat Inap Standar (KRIS) [Perspectives of BPJS Kesehatan Users on the Standard Inpatient Class (KRIS) Policy]. J Jaminan Kesehat Nas DOI: 10.53756/jjkn.v3i1.98.
Maddox KEJ. The Role of Health Policy in Improving Health Outcomes and Health Equity. Trans Am Clin Climatol Assoc 2024; 134: 200–213. https://pmc.ncbi.nlm.nih.gov/articles/PMC11316889/
Alkayyis MY. Implementation of the National Health Insurance Programme in Achieving Universal Health Coverage in Indonesia. J Jaminan Kesehat Nas 2024; 4: 85–95 DOI: 10.53756/jjkn.v4i2.197.
Suryapuspita M. Kebijakan Penyetaraan Kedudukan Sosial Masyarakat melalui Penghapusan Kelas dalam BPJS Kesehatan [The Relationship Between Health Service Coverage and BPJS Class with Estimated Fetal Weight in Pregnant Women: A Retrospective Cross-Sectional Study]. JAPS. https://www.ejurnalskalakesehatan-poltekkesbjm.com/index.php/JSK/article/view/469
Ariyanti AT, Aisyah S. Konflik Norma UU BPJS 2011 dengan UU SJSN 2004 dalam Sistem Jaminan Sosial. J Huk dan Etika Kesehat 2025; 88–102. https://jhek.hangtuah.ac.id/index.php/jurnal/article/download/254/61
Handojo P, Hawadi LF, Lestari HM. A study on the impact of the Standard Inpatient Class (KRIS) policy on private hospitals in Central Jakarta. JHeS (Journal Heal Stud 2025; 9: 50–62.
Gaffar AA, Mayansara A, Zalumin. Operational and Financial Barriers in KRIS Implementation: A Critical Review of Hospital Readiness and Equity in Indonesia. Int J Sci Technol Heal; 3. Epub ahead of print 30 July 2025. DOI: 10.63441/ijsth.v3i2.33.
Saputri NS, Darmawan AB, Toyamah N, et al. Political Economy Analysis of Health Financing Reforms in Times of Crisis: Identifying Windows of Opportunity for Countries in the SEA Region. Indonesia Case Study Report., www.smeru.or.id. (2024). https://smeru.or.id/sites/default/files/publication/political_economy_analysis_of_health_financing_reforms_in_times_of_crisis_smeru.pdf
Imtihani H, Nasser M. Keadilan dalam Reformasi BPJS: Teori Rawls dan Kajian Kritis Terhadap Kebijakan Kelas Rawat Inap Standar [Justice in BPJS Reform: Rawls’ Theory and a Critical Review of the Standardized Inpatient Class Policy]. Syntax Idea 2024; 6: 3832–3842. DOI: 10.46799/syntax-idea.v6i9.4447
Obienyem V, Nweke C. John Rawls’ Theory of Justice: Relevance to Nigeria Ethno-Religious Challenges. JurnalFsUmiAcId 2024; 2: 203–214. http://103.133.36.82/index.php/alpamet/article/view/862
Sidiq Himawan NS. Literature Review: Analysis of Hospital Readiness in Facing Standard Inpatient Class (Kris). Pharmacol Med Reports Orthop Illn Details 2024; 3: 7–19. https://journals.indexcopernicus.com/api/file/viewByFileId/1988359
Natalia C. Hubungan Miskonsepsi Publik Terhadap Isu Penghapusan Kelas BPJS Kesehatan dengan Belum Baiknya “Tata Kelola Yang Baik.” [The Correlation between Public Misconceptions about The Class Abolishment of BPJS Kesehatan and Bad sign of the “Good Governance” system]. https://www.researchgate.net/publication/357364111_HUBUNGAN_MISKONSEPSI_PUBLIK_TERHADAP_ISU_PENGHAPUSAN_KELAS_BPJS_KESEHATAN_DENGAN_BELUM_BAIKNYA_TATA_KELOLA_YANG_BAIK
Rosyidah. Evaluation of the Implementation of the Indonesia Social Insurance Model of Health Care. https://pure.coventry.ac.uk/ws/portalfiles/portal/53327245/2022_Rosyidah_PhD.pdf
Raisha Syahidah, Meutya Zahra Eriansyah, Riswandy Wasir. Inovasi Pendanaan Kesehatan untuk Mewujudkan UHC di Indonesia : Literature Review. J Ilm Kedokt dan Kesehat 2025; 4: 99–106. https://www.researchgate.net/publication/391371698_Inovasi_Pendanaan_Kesehatan_untuk_Mewujudkan_UHC_di_Indonesia_Literature_Review
Alayed TM, Alrumeh AS, Alkanhal IA, et al. Impact of Privatization on Healthcare System: A Systematic Review. Saudi J Med Med Sci 2024; 12: 125–133. DOI: 10.4103/sjmms.sjmms_510_23
Fajarwati, Muchlis, Batara S. Faktor Internal dan Eksternal Kesiapan Masyarakat Tentang Rencana Kebijakan Keseragaman Kelas BPJS [Internal and External Factors of Community Readiness Regarding the Planned Policy of BPJS Class Standardization]. J Mirai Manag. https://journal.stieamkop.ac.id/index.php/mirai/article/view/5210
Hakiki BA. Analysis of the Review of the Standard Inpatient Class Policy (KRIS) as a Replacement for the BPJS Health Class System in Improving Health Service Equity Based on Presidential Regulation Number 59 of 2024. Int J Soc Welf Fam Law 2025; 2: 33–46.DOI: 10.62951/ijsw.v2i1.157
Salisu M, Marquez C, Jha A, et al. A Qualitative Exploration of Barriers and Enablers to Health Equity Competencies in Clinical Practice: Application of the Health Equity Implementation Framework. J Prim Care Community Health 2025; 16: 21501319251363660. DOI: 10.1177/21501319251363661
Sartini M, Carbone A, Demartini A, et al. Overcrowding in Emergency Department: Causes, Consequences, and Solutions—A Narrative Review. Healthcare 2022; 10: 1625. DOI: 10.3390/healthcare10091625
Paek SC, Zhang NJ. Determinants of the low use of Thailand’s Universal Coverage Scheme: a national cross-sectional study. Front Public Heal; 12. Epub ahead of print 22 November 2024. DOI: 10.3389/fpubh.2024.1475319
Mahendradhata Y, Andayani NLPE, Hasri ET, et al. The Capacity of the Indonesian Healthcare System to Respond to COVID-19. Front public Heal 2021; 9: 649819. DOI: 10.3389/fpubh.2021.649819
Salisbury L, Baraitser L, Catty J, et al. A waiting crisis? Lancet (London, England) 2023; 401: 428–429. DOI: 10.1016/S0140-6736(23)00238-6
Copyright (c) 2025 Daniel Pradana Andrian Wicaksono

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.