Determinants of Postpartum Blues in Indonesia
Downloads
Introduction: The condition of postpartum blues is difficult to detect as it is still considered an instinct from a mother. Postpartum blues is a psychiatric disorder that, if left untreated, causes severe mental problems. This study aims to determine the factors that influences postpartum blues in postpartum mothers.
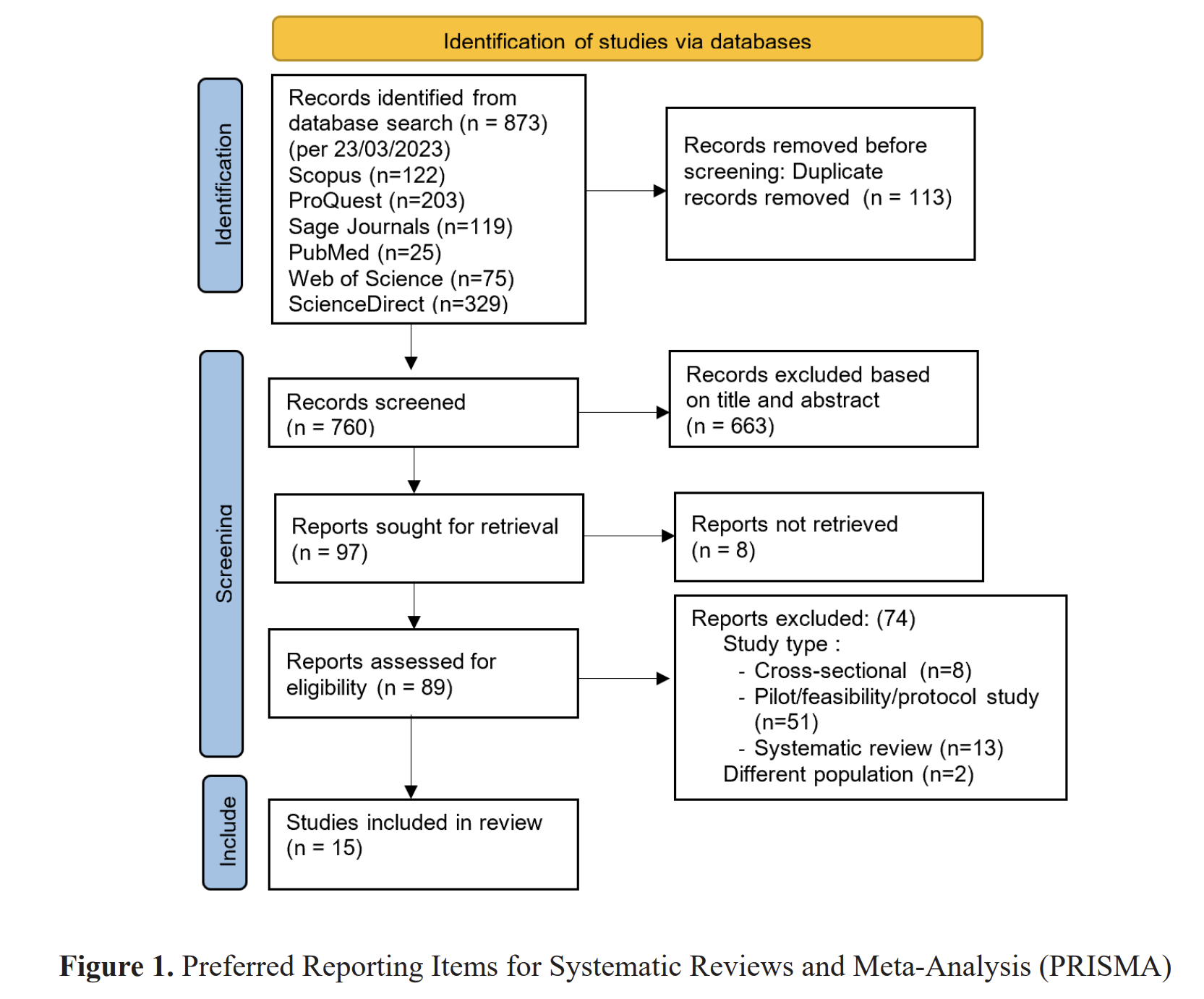
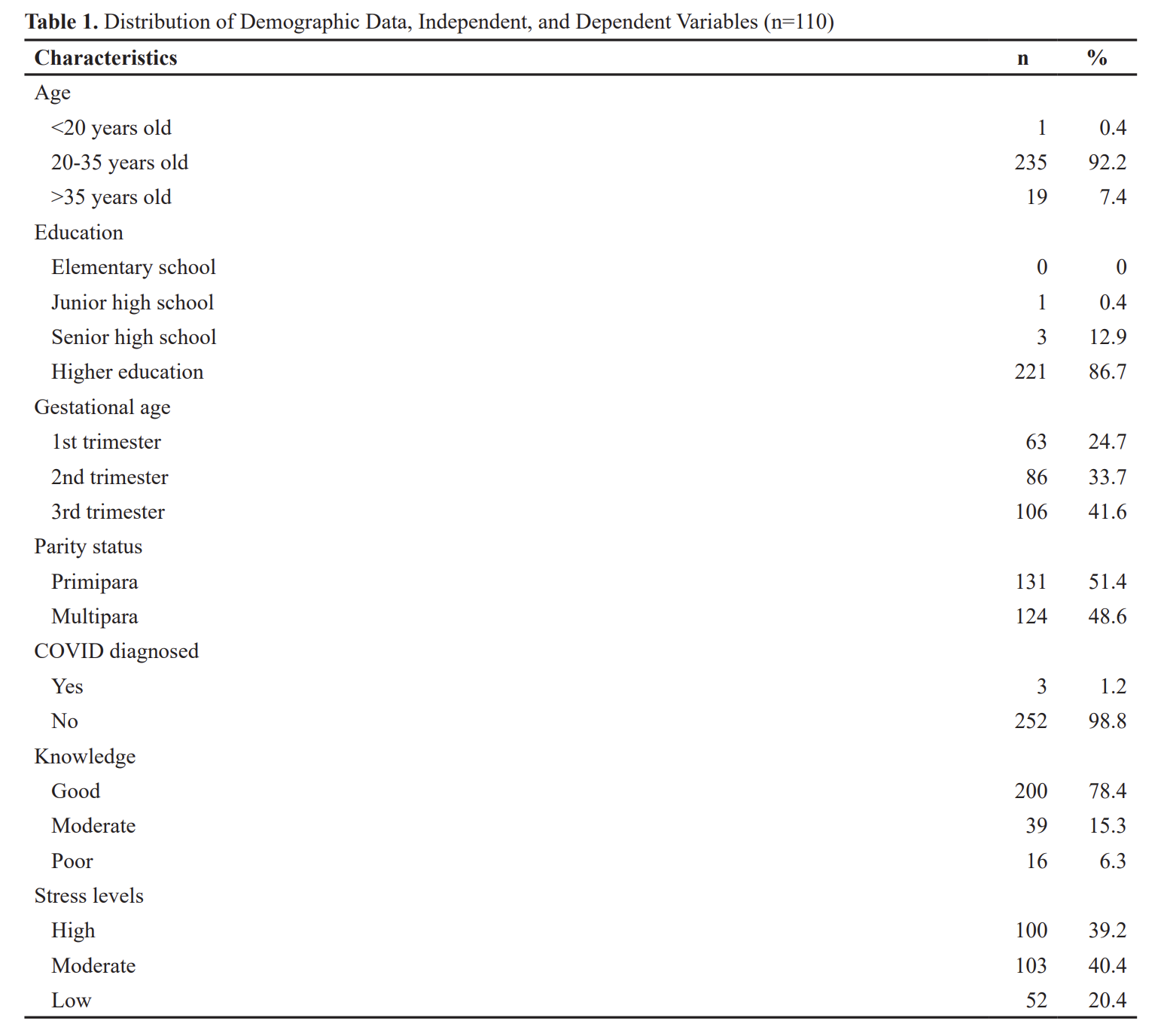
Methods: This study used a cross-sectional method. The population in this study were mothers who gave birth at Balung Hospital. The sample obtained were 330 mothers who gave birth from January to December 2019. The instrument used was a questionnaire consisting of the Edinburgh Postnatal Depression Scale, a family support questionnaire, and a questionnaire to determine the respondent's characteristic data (age, salary, education, employment, type of labor, husband support, pregnancy status, and risk of postpartum blues)
Results: The results of the analysis using the chi-square found that the determinants of postpartum blues are age (p=0.002), salary (p=0.032), education (p=0.001), occupation (p=0.042), type of delivery (p=0.0001), husband's support (p=0.003), and pregnancy status (p=0.009) with p <0.05.
Conclusion: Mothers who receive the related factors will feel that they are valuable and needed and therefore a sense of happiness and comfort will arise to improve the mother's mood. Health workers can support the factors that promote the reduction of the postpartum blues status.
Aaronson, B. D. (2010). Parental bonding memories, adult attachment, interpersonal problems, and perceptions of maternal depression. Fordham University.
Bernstein, H. H., Spino, C., Lalama, C. M., Finch, S. A., Wasserman, R. C., & McCormick, M. C. (2013). Unreadiness for postpartum discharge following healthy term pregnancy: impact on health care use and outcomes. Academic Pediatrics, 1;13(1):27. https://doi.org/10.1016/j.acap.2012.08.005
Connelly, M., Brown, H., Pligt, P., & Teychenne, M. (2015). Modifiable barriers to leisure-time physical activity during pregnancy: a qualitative study investigating first time mother's views and experiences. BMC Pregnancy and Childbirth, 1;15(1):10. https://dx.doi.org/10.1186%2Fs12884-015-0529-9
Denis, A., Ponsin, M., & Callahan, S. (2012). The relationship between maternal self-esteem, maternal competence, infant temperament and post-partum blues. Journal of Reproductive and Infant Psychology, 1;30(4):38. https://doi.org/10.1080/02646838.2012.718751
Dowlati, Y., Segal, Z. V, Ravindran, A. V, Steiner, M., Stewart, D. E., & Meyer, J. H. (2014). Effect of dysfunctional attitudes and postpartum state on vulnerability to depressed mood. Journal of Affective Disorders, 161, 16–20. https://doi.org/10.1016/j.jad.2014.02.047
Fall, C. H., Sachdev, H. S., Osmond, C., Restrepo-Mendez, M. C., Victora, C., Martorell, R., Stein, A. D., Sinha, S., Tandon, N., Adair, L., & Bas, I. (2012). Association between maternal age at childbirth and child and adult outcomes in the offspring: a prospective study in five low-income and middle-income countries (COHORTS collaboration. The Lancet Global Health, 1;3(7):e36. https://doi.org/10.1016/s2214-109x(15)00038-8
Gaillard, A., Le Strat, Y., Mandelbrot, L., Keita, H., & Dubertret, C. (2014). Predictors of postpartum depression: prospective study of 264 women followed during pregnancy and postpartum. Psychiatry Research, 28;215(2): https://doi.org/10.1016/j.psychres.2013.10.003
Goecke, T. W., Voigt, F., Faschingbauer, F., Spangler, G., Beckmann, M. W., & Beetz, A. (2012). The association of prenatal attachment and perinatal factors with pre-and postpartum depression in first-time mothers. Archives of Gynecology and Obstetrics, 1;286(2):3. https://doi.org/10.1007/s00404-012-2286-6
Karabulut, A., Ozkan, S., Bozkurt, A. I., Karahan, T., & Kayan, S. (2013). Perinatal outcomes and risk factors in adolescent and advanced age pregnancies: comparison with normal reproductive age women. Journal of Obstetrics and Gynaecology, 1;33(4):34. http://dx.doi.org/10.3109/01443615.2013.767786
Kathree, T., Selohilwe, O. M., Bhana, A., & Petersen, I. (2014). Perceptions of postnatal depression and health care needs in a South African sample: the "mental” in maternal health care. BMC Women's Health, 1;14(1):14. https://doi.org/10.1186/s12905-014-0140-7
Kingston, D., Heaman, M., Fell, D., & Chalmers, B. (2012). Maternity Experiences Study Group of the Canadian Perinatal Surveillance System. Comparison of adolescent, young adult, and adult women's maternity experiences and practices. Pediatrics, 1;129(5):e. https://doi.org/10.1542/peds.2011-1447
Lanes, A., Kuk, J. L., & Tamim, H. (2011). Prevalence and characteristics of postpartum depression symptomatology among Canadian women: a cross-sectional study. BMC Public Health, 1;11(1):30. https://doi.org/10.1186/1471-2458-11-302
Leahy"Warren, P., McCarthy, G., & Corcoran, P. (2012). First"time mothers: social support, maternal parental self"efficacy and postnatal depression. Journal of Clinical Nursing, Feb;21(3"4. https://doi.org/10.1111/j.1365-2702.2011.03701.x
Lee, S. L., Liu, C. Y., Lu, Y. Y., & Gau, M. L. (2013). Efficacy of warm showers on labor pain and birth experiences during the first labor stage. Journal of Obstetric, Gynecologic & Neonatal Nursing, 1;42(1):19. https://doi.org/10.1111/j.1552-6909.2012.01424.x
Manurung, S., Setyowati, S., Ginanjar, A. S., Soesilo, T. E., & Tyastuti, D. (2019). The Item Development of Maternal Blues Suryani (MBS) Scale in the antepartum period through bonding attachment that predicting postpartum blues. Enfermeria Clinica, 29, 752–9. https://doi.org/10.1016/j.enfcli.2019.06.013
McKelvey, M. M., & Espelin, J. (2018). Postpartum depression: Beyond the "baby blues.” Nursing Made Incredibly Easy, 1;16(3):28. https://doi.org/10.1097/01.NME.0000531872.48283.ab
Negron, R., Martin, A., Almog, M., Balbierz, A., & Howell, E. A. (2013). Social support during the postpartum period: mothers' views on needs, expectations, and mobilization of support. Maternal and Child Health Journal, 1;17(4):61. https://doi.org/10.1007/s10995-012-1037-4
Nilaweera, I., Doran, F., & Fisher, J. (2014). Prevalence, nature and determinants of postpartum mental health problems among women who have migrated from South Asian to high-income countries: a systematic review of the evidence. Journal of Affective Disorders, 166, 213–26. https://doi.org/10.1016/j.jad.2014.05.021
Orchard, C. A. (2010). Persistent isolationist or collaborator? The nurse's role in interprofessional collaborative practice. Journal of Nursing Management, Apr;18(3): https://doi.org/10.1111/j.1365-2834.2010.01072.x
Pope, C. J., & Mazmanian, D. (2016). Breastfeeding and postpartum depression: an overview and methodological recommendations for future research. Depression Research and Treatment. https://doi.org/10.1155/2016/4765310
Razurel, C., Bruchon-Schweitzer, M., Dupanloup, A., Irion, O., & Epiney, M. (2011). Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery, Apr 1;27(2. https://doi.org/10.1016/j.midw.2009.06.005
Rouhi, M., S, M. C., Usefi, H., & Rouhi, N. (2011). Postpartum morbidity and help-seeking behaviours in Iran. British Journal of Midwifery, Mar;19(3): https://doi.org/10.12968/bjom.2011.19.3.178
Smith, D. W., Sawyer, G. K., Jones, L. M., Cross, T., McCart, M. R., & Ralston, M. E. (2010). Mother reports of maternal support following child sexual abuse: Preliminary psychometric data on the Maternal Self-report Support Questionnaire (MSSQ. Child Abuse & Neglect, 1;34(10):7. http://dx.doi.org/10.1016/j.chiabu.2010.02.009
Sparks R. Sadness and Support: A Short History of Postpartum Depression. (2013). Mary Becker Rysavy Essay Contest-UI Carver College of Medicine.
Usdansky, M. L., Gordon, R. A., Wang, X., & Gluzman, A. (2012). Depression risk among mothers of young children: The role of employment preferences, labor force status and job quality. Journal of Family and Economic Issues, 1;33(1):83. http://dx.doi.org/10.1007/s10834-011-9260-5
Wang, L., Wu, T., Anderson, J. L., & Florence, J. E. (2011). Prevalence and risk factors of maternal depression during the first three years of child rearing. Journal of Women's Health, 1;20(5):71. https://doi.org/10.1089/jwh.2010.2232
Zhong, Q. Y., Gelaye, B., Rondon, M. B., Sánchez, S. E., Simon, G. E., Henderson, D. C., Barrios, Y. V, Sánchez, P. M., & Williams, M. A. (2015). Using the Patient Health Questionnaire (PHQ-9) and the Edinburgh Postnatal Depression Scale (EPDS) to assess suicidal ideation among pregnant women in Lima, Peru. Archives of Women's Mental Health, 1;18(6):78. https://doi.org/10.1007/s00737-014-0481-0
Zhu, P., Tao, F., Hao, J., Sun, Y., & Jiang, X. (2010). Prenatal life events stress: implications for preterm birth and infant birthweight. American Journal of Obstetrics and Gynecology, 1;203(1):3. https://doi.org/10.1016/j.ajog.2010.02.023
Copyright (c) 2021 Eka Afdi Septiyono, Dini Kurniawati

This work is licensed under a Creative Commons Attribution 4.0 International License.
1. The journal allows the author to hold the copyright of the article without restrictions.
2. The journal allows the author(s) to retain publishing rights without restrictions.
3. The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution (CC BY).