Main Article Content
Abstract
Highlights:
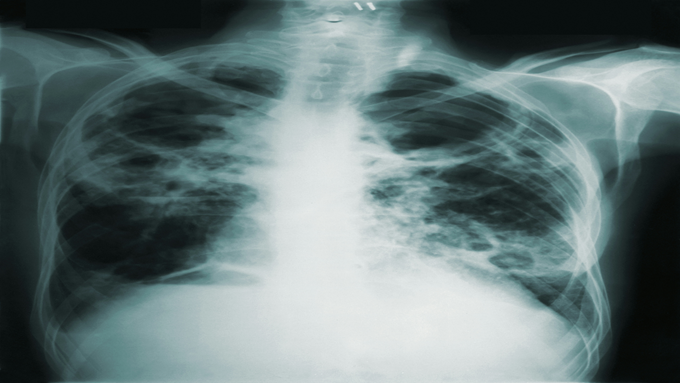
1. This study was the first in Gresik, Indonesia, to conduct mass screening of tuberculosis among waste workers, comprising various demographic profiles.
2. Although the tuberculosis screening of the waste workers showed negative results, mass examination using an acid-fast bacilli smear remains crucial to detect latent infections and prevent transmissions.
Abstract
Tuberculosis is a major source of illness and mortality worldwide. Therefore, tuberculosis screening is important to increase the number of active case-finding in a community. Bacteriological examinations can be used to initiate community-based active case-finding. Waste workers face a high risk of contracting Mycobacterium tuberculosis due to their constant exposure to waste. This study aimed to conduct bacteriological examinations to identify tuberculosis infections among waste workers in Gresik, Indonesia, who were considered a high-risk group. An analytical observational study was carried out throughout September 2023 in the Ngipik subdistrict, Gresik, East Java, Indonesia. The primary study was conducted using a cross-sectional design using interviews, measurements, and sputum examinations for all samples. The screening involved a total of 72 waste workers who had daily contact with various types of sewage and waste, including medical waste. The data were analyzed descriptively because of the constant variable. Following the analysis, the data were presented using a table and a figure. According to the acid-fast bacilli examinations, all of the samples yielded negative results. Nevertheless, this study concludes that it is imperative to carry out mass tuberculosis screening in various settings, specifically among those with a high risk. Mass screening can uncover the potential of latent tuberculosis and, thus, reduce its transmission.
Keywords
Article Details
Copyright (c) 2024 Folia Medica Indonesiana

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
-
Folia Medica Indonesiana is a scientific peer-reviewed article which freely available to be accessed, downloaded, and used for research purposes. Folia Medica Indonesiana (p-ISSN: 2541-1012; e-ISSN: 2528-2018) is licensed under a Creative Commons Attribution 4.0 International License. Manuscripts submitted to Folia Medica Indonesiana are published under the terms of the Creative Commons License. The terms of the license are:
Attribution ” You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
NonCommercial ” You may not use the material for commercial purposes.
ShareAlike ” If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
No additional restrictions ” You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
You are free to :
Share ” copy and redistribute the material in any medium or format.
Adapt ” remix, transform, and build upon the material.

References
- Advisory Committee on Dangerous Pathogens (2003). Infection at work: Controlling the risk. Norwich. Available at: http://www.fiocruz.br/bios seguranca/Bis/manuais/biosseguranca/infection_at_work_controlling_the_risks.pdf.
- Andajani S (2019). Determinant of latent pulmonary tuberculosis incidence among health workers in community health centers in Surabaya, Indonesia. Folia Medica Indonesiana 55, 139. doi: 10.20473/ fmi.v55i2.14348.
- ArcGIS Desktop (2018). ArcGIS fow windows, version 10.6. Esri, Redlands, CA, USA. Available at: https://arcgis.software.informer.com/10.6/
- Bagherirad M, Trevan P, Globan M, et al (2014). Transmission of tuberculosis infection in a commercial office. Medical Journal of Australia 200, 177–179. doi: 10.5694/mja12.11750.
- Baral YR (2018). Waste workers and occupational health risks. International Journal of Occupational Safety and Health 8, 1–3. doi: 10.3126/ijosh.v8i2. 23328.
- Campelo TA, Cardoso de Sousa PR, Nogueira L de L, et al (2021). Revisiting the methods for detecting Mycobacterium tuberculosis: what has the new millennium brought thus far?. Access Microbiology. doi: 10.1099/acmi.0.000245.
- Centers for Disease Control and Prevention (2022). Tuberculosis. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/tb/ default.htm.
- Chakaya J, Khan M, Ntoumi F, et al (2021). Global tuberculosis report 2020: Reflections on the global TB burden, treatment and prevention efforts. International Journal of Infectious Diseases 113, 7–12. doi: 10.1016/j.ijid.2021.02.107.
- Chandra K, Arora VK (2019). Tuberculosis and other chronic morbidity profile of sewage workers of Delhi. Indian Journal of Tuberculosis 66, 144–149. doi: 10.1016/j.ijtb.2018.09.003.
- Han J, He S, Shao W, et al (2023). Municipal solid waste, an overlooked route of transmission for the severe acute respiratory syndrome coronavirus 2: A review. Environmental Chemistry Letters 21, 81–95. doi: 10.1007/s10311-022-01512-y.
- Hapsari BAP, Wulaningrum PA, Rimbun R (2021). Association between smoking habit and pulmonary tuberculosis at Dr. Soetomo General Academic Hospital. Biomolecular and Health Science Journal 4, 89. doi: 10.20473/bhsj.v4i2.30 641.
- Hickey AJ, Cummings MJ, Zafari Z, et al (2022). Evaluation of screening strategies for pulmonary tuberculosis among hospitalized patients in a low-burden setting: Cost-effectiveness of GeneXpert MTB/RIF compared to smear microscopy. Infection Control & Hospital Epidemiology 43, 892–897. doi: 10.1017/ice.2021.247.
- Hopewell PC, Pai M, Maher D, et al (2006). International standards for tuberculosis care. The Lancet Infectious Diseases 6, 710–725. doi: 10.1016/S1473-3099(06)70628-4.
- Hu Z, Liu K, Zhou M, et al (2023). Mass tuberculosis screening among the elderly: A population-based study in a well-confined, rural county in Eastern China. Clinical Infectious Diseases 77, 1468–1475. doi: 10.1093/cid/ciad 438.
- Lakoh S, Jiba DF, Adekanmbi O, et al (2020). Diagnosis and treatment outcomes of adult tuberculosis in an urban setting with high HIV prevalence in Sierra Leone: A retrospective study. International Journal of Infectious Diseases 96, 112–118. doi: 10.1016/j.ijid.2020.04.038.
- Ministry of Health of the Republic of Indonesia (2022). Dashboard tuberculosis. Ministry of Health of the Republic of Indonesia. Available at: https://tbindonesia.or.id/dashboard-tb-indonesia/.
- Ngabonziza JCS, Ssengooba W, Mutua F, et al (2016). Diagnostic performance of smear microscopy and incremental yield of Xpert in detection of pulmonary tuberculosis in Rwanda. BMC Infectious Diseases 16, 660. doi: 10.1186/s1 2879-016-2009-x.
- Nicolini A, Grecchi B, Ferrari-Bravo M, et al (2018). Safety and effectiveness of the high-frequency chest wall oscillation vs intrapulmonary percussive ventilation in patients with severe COPD. International Journal of Chronic Obstructive Pulmonary Disease 13, 617–625. doi: 10.2147/COPD.S145440.
- Ranganathan P, Aggarwal R (2019). Study designs: Part 3 - Analytical observational studies. Perspectives in Clinical Research 10, 91. doi: 10.4103/picr.PICR_35_19.
- Schluger NW (2019). The acid-fast bacilli smear: Hail and farewell. American Journal of Respiratory and Critical Care Medicine 199, 691–692. doi: 10.1164/rccm.201809-1772ED.
- Shiferaw MB, Hailu HA, Fola AA, et al (2015). Tuberculosis laboratory diagnosis quality assurance among public health facilities in West Amhara Region, Ethiopia. PLoS One 10. doi: 10.1371/journal.pone.0138488.
- Sreeramareddy CT, Panduru K V, Menten J, et al (2009). Time delays in diagnosis of pulmonary tuberculosis: A systematic review of literature. BMC Infectious Diseases 9, 91. doi: 10.1186/ 1471-2334-9-91.
- Syahputri SAH, Mufida DC, Bumi C (2023). Epidemiology of pulmonary tuberculosis in diabetes mellitus patients. Jurnal Kesehatan 14, 345. doi: 10.26630/jk.v14i2.3963.
- Weber AM, Boudreau Y, Mortimer VD (2000). A tuberculosis outbreak among medical waste workers. Journal of the American Biological Safety Association 5, 70–88. doi: 10.1177/109135 050000500207.
- World Health Organization (2017). Global investments in tuberculosis research and development: Past, present and future. A policy paper prepared for the first WHO global ministerial conference on ending tuberculosis in the sustainable development era: A multisectoral response. WHO. Available at: https://www.who. int/publications/i/item/9789241513326.
- World Health Organization (2018). Smoking and tuberculosis: A dangerous combination. WHO. Available at: https://www.who.int/europe/news/ item/22-03-2018-smoking-and-tuberculosis-a-dangerous-combination.
- World Health Organization (2022). The end TB strategy. WHO. Available at: https://www.who. int/teams/global-tuberculosis-programme/the-end -tb-strategy.
- Zamudio C, Krapp F, Choi HW, et al (2015). Public transportation and tuberculosis transmission in a high incidence setting ed. Mokrousov I. PLoS One 10. doi: 10.1371/journal.pone.0115230.
References
Advisory Committee on Dangerous Pathogens (2003). Infection at work: Controlling the risk. Norwich. Available at: http://www.fiocruz.br/bios seguranca/Bis/manuais/biosseguranca/infection_at_work_controlling_the_risks.pdf.
Andajani S (2019). Determinant of latent pulmonary tuberculosis incidence among health workers in community health centers in Surabaya, Indonesia. Folia Medica Indonesiana 55, 139. doi: 10.20473/ fmi.v55i2.14348.
ArcGIS Desktop (2018). ArcGIS fow windows, version 10.6. Esri, Redlands, CA, USA. Available at: https://arcgis.software.informer.com/10.6/
Bagherirad M, Trevan P, Globan M, et al (2014). Transmission of tuberculosis infection in a commercial office. Medical Journal of Australia 200, 177–179. doi: 10.5694/mja12.11750.
Baral YR (2018). Waste workers and occupational health risks. International Journal of Occupational Safety and Health 8, 1–3. doi: 10.3126/ijosh.v8i2. 23328.
Campelo TA, Cardoso de Sousa PR, Nogueira L de L, et al (2021). Revisiting the methods for detecting Mycobacterium tuberculosis: what has the new millennium brought thus far?. Access Microbiology. doi: 10.1099/acmi.0.000245.
Centers for Disease Control and Prevention (2022). Tuberculosis. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/tb/ default.htm.
Chakaya J, Khan M, Ntoumi F, et al (2021). Global tuberculosis report 2020: Reflections on the global TB burden, treatment and prevention efforts. International Journal of Infectious Diseases 113, 7–12. doi: 10.1016/j.ijid.2021.02.107.
Chandra K, Arora VK (2019). Tuberculosis and other chronic morbidity profile of sewage workers of Delhi. Indian Journal of Tuberculosis 66, 144–149. doi: 10.1016/j.ijtb.2018.09.003.
Han J, He S, Shao W, et al (2023). Municipal solid waste, an overlooked route of transmission for the severe acute respiratory syndrome coronavirus 2: A review. Environmental Chemistry Letters 21, 81–95. doi: 10.1007/s10311-022-01512-y.
Hapsari BAP, Wulaningrum PA, Rimbun R (2021). Association between smoking habit and pulmonary tuberculosis at Dr. Soetomo General Academic Hospital. Biomolecular and Health Science Journal 4, 89. doi: 10.20473/bhsj.v4i2.30 641.
Hickey AJ, Cummings MJ, Zafari Z, et al (2022). Evaluation of screening strategies for pulmonary tuberculosis among hospitalized patients in a low-burden setting: Cost-effectiveness of GeneXpert MTB/RIF compared to smear microscopy. Infection Control & Hospital Epidemiology 43, 892–897. doi: 10.1017/ice.2021.247.
Hopewell PC, Pai M, Maher D, et al (2006). International standards for tuberculosis care. The Lancet Infectious Diseases 6, 710–725. doi: 10.1016/S1473-3099(06)70628-4.
Hu Z, Liu K, Zhou M, et al (2023). Mass tuberculosis screening among the elderly: A population-based study in a well-confined, rural county in Eastern China. Clinical Infectious Diseases 77, 1468–1475. doi: 10.1093/cid/ciad 438.
Lakoh S, Jiba DF, Adekanmbi O, et al (2020). Diagnosis and treatment outcomes of adult tuberculosis in an urban setting with high HIV prevalence in Sierra Leone: A retrospective study. International Journal of Infectious Diseases 96, 112–118. doi: 10.1016/j.ijid.2020.04.038.
Ministry of Health of the Republic of Indonesia (2022). Dashboard tuberculosis. Ministry of Health of the Republic of Indonesia. Available at: https://tbindonesia.or.id/dashboard-tb-indonesia/.
Ngabonziza JCS, Ssengooba W, Mutua F, et al (2016). Diagnostic performance of smear microscopy and incremental yield of Xpert in detection of pulmonary tuberculosis in Rwanda. BMC Infectious Diseases 16, 660. doi: 10.1186/s1 2879-016-2009-x.
Nicolini A, Grecchi B, Ferrari-Bravo M, et al (2018). Safety and effectiveness of the high-frequency chest wall oscillation vs intrapulmonary percussive ventilation in patients with severe COPD. International Journal of Chronic Obstructive Pulmonary Disease 13, 617–625. doi: 10.2147/COPD.S145440.
Ranganathan P, Aggarwal R (2019). Study designs: Part 3 - Analytical observational studies. Perspectives in Clinical Research 10, 91. doi: 10.4103/picr.PICR_35_19.
Schluger NW (2019). The acid-fast bacilli smear: Hail and farewell. American Journal of Respiratory and Critical Care Medicine 199, 691–692. doi: 10.1164/rccm.201809-1772ED.
Shiferaw MB, Hailu HA, Fola AA, et al (2015). Tuberculosis laboratory diagnosis quality assurance among public health facilities in West Amhara Region, Ethiopia. PLoS One 10. doi: 10.1371/journal.pone.0138488.
Sreeramareddy CT, Panduru K V, Menten J, et al (2009). Time delays in diagnosis of pulmonary tuberculosis: A systematic review of literature. BMC Infectious Diseases 9, 91. doi: 10.1186/ 1471-2334-9-91.
Syahputri SAH, Mufida DC, Bumi C (2023). Epidemiology of pulmonary tuberculosis in diabetes mellitus patients. Jurnal Kesehatan 14, 345. doi: 10.26630/jk.v14i2.3963.
Weber AM, Boudreau Y, Mortimer VD (2000). A tuberculosis outbreak among medical waste workers. Journal of the American Biological Safety Association 5, 70–88. doi: 10.1177/109135 050000500207.
World Health Organization (2017). Global investments in tuberculosis research and development: Past, present and future. A policy paper prepared for the first WHO global ministerial conference on ending tuberculosis in the sustainable development era: A multisectoral response. WHO. Available at: https://www.who. int/publications/i/item/9789241513326.
World Health Organization (2018). Smoking and tuberculosis: A dangerous combination. WHO. Available at: https://www.who.int/europe/news/ item/22-03-2018-smoking-and-tuberculosis-a-dangerous-combination.
World Health Organization (2022). The end TB strategy. WHO. Available at: https://www.who. int/teams/global-tuberculosis-programme/the-end -tb-strategy.
Zamudio C, Krapp F, Choi HW, et al (2015). Public transportation and tuberculosis transmission in a high incidence setting ed. Mokrousov I. PLoS One 10. doi: 10.1371/journal.pone.0115230.