Early Management of Aspiration Pneumonia in an Infant With Suspected Laryngomalacia in A Resource-Limited Setting: A Case Report
Downloads
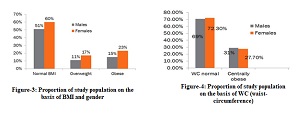
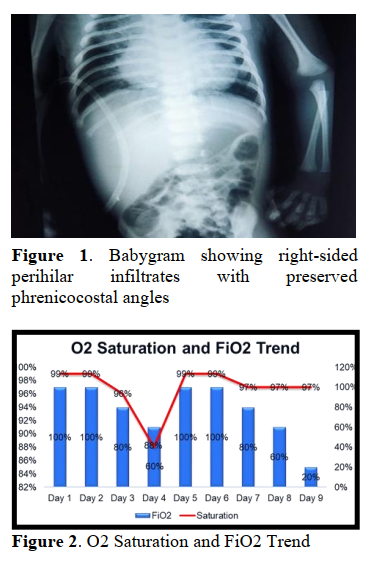
Laryngomalacia is the most common cause of congenital stridor in infants and can lead to feeding difficulties, failure to thrive, and respiratory distress. Diagnosis typically requires flexible fiberoptic laryngoscopy, which more often than not, not available in resource-limited settings. We report a 12-day-old male infant who presented to the emergency department with apnea following a choking episode. He required cardiopulmonary resuscitation and was admitted to the neonatal intensive care unit. Clinical findings included chest retractions, cyanosis, weight loss (from 3500g at birth to 2700g), and feeding difficulties. Chest radiograph showed right-sided perihilar infiltrates consistent with aspiration pneumonia. Despite initial clinical improvement, the infant developed new-onset positional stridor on day ten of hospitalization, particularly when supine. These findings raised strong suspicion of underlying laryngomalacia. These signs raised a strong clinical suspicion of laryngomalacia. Due to absence of flexible fiberoptic laryngoscopy, diagnosis could not be confirmed. The infant was stabilised with supportive care and feeding adjustments before being referred to a tertiary center for definitive evaluation and management. This case highlights the importance of prompt recognition and early stabilisation of neonates with aspiration-related complications and suspected airway anomalies, particularly in low-resource settings. Timely referral is essential to prevent deterioration and guide appropriate long-term management.
Thorne MC, Garetz SL. Laryngomalacia : Review and Summary of Current Clinical Practice in 2015. Paediatric Respiratory Reviews. 2015; DOI: 10.1016/j.prrv.2015.02.002
Bedwell J, Zalzal G. Laryngomalacia. Seminars in Pediatric Surgery. 2016;25(3):119–22. DOI: 10.1053/j.sempedsurg.2016.02.004
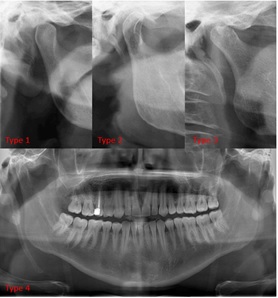
Kusak B, Cichocka-Jarosz E, Jedynak-Wasowicz U, Lis G. Types of laryngomalacia in children: interrelationship between clinical course and comorbid conditions. European Archives of Oto-Rhino-Laryngology. 2017;274(3):1577–83. DOI: 10.1007/s00405-016-4334-5
Parkes WJ, Propst EJ. Advances in the diagnosis, management, and treatment of neonates with laryngeal disorders. Seminars in Fetal and Neonatal Medicine. 2016 Aug 1;21(4):270–6. DOI: 10.1016/j.siny.2016.03.003
Klinginsmith M, Winters R, Goldman J. Laryngomalacia. StatPearls [Internet]. 2024; https://www.ncbi.nlm.nih.gov/books/NBK544266/
Irace AL, Dombrowski ND, Kawai K, Watters K, Choi S, Perez J, et al. Evaluation of Aspiration in Infants With Laryngomalacia and Recurrent Respiratory and Feeding Difficulties. JAMA Otolaryngology–Head & Neck Surgery [Internet]. 2019 Feb 1 [cited 2025 Jul 17];145(2):146–51. DOI: 10.1001/jamaoto.2018.3642
Bowman OJ, Hagan JL, Toruno RM, Wiggin MM. Identifying Aspiration Among Infants in Neonatal Intensive Care Units Through Occupational Therapy Feeding Evaluations. The American Journal of Occupational Therapy [Internet]. 2020 Feb 1 [cited 2025 Jul 17];74(1):7401205080p1. DOI: 10.5014/ajot.2020.022137
Landry AM, Thompson DM. Laryngomalacia: Disease Presentation, Spectrum, and Management. International Journal of Pediatrics. 2012;2012:1–6. DOI: 10.1155/2012/753526
Jaffal H, Isaac A, Johannsen W, Campbell S, El-Hakim HG. The prevalence of swallowing dysfunction in children with laryngomalacia: a systematic review. International Journal of Pediatric Otorhinolaryngology. 2020 Dec 1;139:110464. DOI: 10.1016/j.ijporl.2020.110464
Irace AL, Dombrowski ND, Kawai K, Watters K, Choi S, Perez J, et al. Evaluation of Aspiration in Infants with Laryngomalacia and Recurrent Respiratory and Feeding Difficulties. JAMA Otolaryngology - Head and Neck Surgery. 2019;145(2):146–51. DOI: 10.1001/jamaoto.2018.3642
Ha JF. Dysphagia in laryngomalacia: a prospective cohort study. Australian Journal of Otolaryngology. 2022;5. DOI: 10.21037/ajo-21-44
Thottam PJ, Simons JP, Choi S, Maguire R, Mehta DK. Clinical relevance of quality of life in laryngomalacia. Laryngoscope. 2016;126(5):1232–5. DOI: 10.1002/lary.25491
Bhatt J, Prager JD. Neonatal Stridor: Diagnosis and Management. Clinics in Perinatology. 2018;45(4):817–31. DOI: 10.1016/j.clp.2018.07.015
Scott BL, Lam D, MacArthur C. Laryngomalacia and 1. Thorne MC, Garetz SL. Laryngomalacia : Review and Summary of Current Clinical Practice in 2015. Paediatric Respiratory Reviews. 2015; DOI: 10.1016/j.prrv.2015.02.002
Bedwell J, Zalzal G. Laryngomalacia. Seminars in Pediatric Surgery. 2016;25(3):119–22. DOI: 10.1053/j.sempedsurg.2016.02.004
Kusak B, Cichocka-Jarosz E, Jedynak-Wasowicz U, Lis G. Types of laryngomalacia in children: interrelationship between clinical course and comorbid conditions. European Archives of Oto-Rhino-Laryngology. 2017;274(3):1577–83. DOI: 10.1007/s00405-016-4334-5
Parkes WJ, Propst EJ. Advances in the diagnosis, management, and treatment of neonates with laryngeal disorders. Seminars in Fetal and Neonatal Medicine. 2016 Aug 1;21(4):270–6. DOI: 10.1016/j.siny.2016.03.003
Klinginsmith M, Winters R, Goldman J. Laryngomalacia. StatPearls [Internet]. 2024; https://www.ncbi.nlm.nih.gov/books/NBK544266/
Irace AL, Dombrowski ND, Kawai K, Watters K, Choi S, Perez J, et al. Evaluation of Aspiration in Infants With Laryngomalacia and Recurrent Respiratory and Feeding Difficulties. JAMA Otolaryngology–Head & Neck Surgery [Internet]. 2019 Feb 1 [cited 2025 Jul 17];145(2):146–51. DOI: 10.1001/jamaoto.2018.3642
Bowman OJ, Hagan JL, Toruno RM, Wiggin MM. Identifying Aspiration Among Infants in Neonatal Intensive Care Units Through Occupational Therapy Feeding Evaluations. The American Journal of Occupational Therapy [Internet]. 2020 Feb 1 [cited 2025 Jul 17];74(1):7401205080p1. DOI: 10.5014/ajot.2020.022137
Landry AM, Thompson DM. Laryngomalacia: Disease Presentation, Spectrum, and Management. International Journal of Pediatrics. 2012;2012:1–6. DOI: 10.1155/2012/753526
Jaffal H, Isaac A, Johannsen W, Campbell S, El-Hakim HG. The prevalence of swallowing dysfunction in children with laryngomalacia: a systematic review. International Journal of Pediatric Otorhinolaryngology. 2020 Dec 1;139:110464. DOI: 10.1016/j.ijporl.2020.110464
Irace AL, Dombrowski ND, Kawai K, Watters K, Choi S, Perez J, et al. Evaluation of Aspiration in Infants with Laryngomalacia and Recurrent Respiratory and Feeding Difficulties. JAMA Otolaryngology - Head and Neck Surgery. 2019;145(2):146–51. DOI: 10.1001/jamaoto.2018.3642
Ha JF. Dysphagia in laryngomalacia: a prospective cohort study. Australian Journal of Otolaryngology. 2022;5. DOI: 10.21037/ajo-21-44
Thottam PJ, Simons JP, Choi S, Maguire R, Mehta DK. Clinical relevance of quality of life in laryngomalacia. Laryngoscope. 2016;126(5):1232–5. DOI: 10.1002/lary.25491
Bhatt J, Prager JD. Neonatal Stridor: Diagnosis and Management. Clinics in Perinatology. 2018;45(4):817–31. DOI: 10.1016/j.clp.2018.07.015
Scott BL, Lam D, MacArthur C. Laryngomalacia and Swallow Dysfunction. Ear, Nose and Throat Journal. 2019;98(10):613–6. DOI: 10.1177/0145561319847459
Leonard JA, Reilly BK. Laryngomalacia in the Premature Neonate. NeoReviews. 2021;22(10). DOI: 10.1542/neo.22-10-e653
Jain D, Jain S. Management of Stridor in Severe Laryngomalacia: A Review Article. Cureus. 2022;14(9). DOI: 10.7759/cureus.29585
Macedo RB, Dias MS, Salazar L, Alexandre P, Viveiros C, Pereira M, et al. Laryngomalacia and failure to thrive – A case report. Journal of Pediatric and Neonatal Individualized Medicine. 2024;13(2):e130202. https://jpnim.com/index.php/jpnim/article/view/e130202
Cohen O, Picard E, Joseph L, Schwartz Y, Sichel JY, Attal P. Supraglottoplasty for severe laryngomalacia. Can we predict success? International Journal of Pediatric Otorhinolaryngology. 2020;138(May):110333. DOI: 10.1016/j.ijporl.2020.110333
Swallow Dysfunction. Ear, Nose and Throat Journal. 2019;98(10):613–6. DOI: 10.1177/0145561319847459
Leonard JA, Reilly BK. Laryngomalacia in the Premature Neonate. NeoReviews. 2021;22(10). DOI: 10.1542/neo.22-10-e653
Jain D, Jain S. Management of Stridor in Severe Laryngomalacia: A Review Article. Cureus. 2022;14(9). DOI: 10.7759/cureus.29585
Macedo RB, Dias MS, Salazar L, Alexandre P, Viveiros C, Pereira M, et al. Laryngomalacia and failure to thrive – A case report. Journal of Pediatric and Neonatal Individualized Medicine. 2024;13(2):e130202. https://jpnim.com/index.php/jpnim/article/view/e130202
Cohen O, Picard E, Joseph L, Schwartz Y, Sichel JY, Attal P. Supraglottoplasty for severe laryngomalacia. Can we predict success? International Journal of Pediatric Otorhinolaryngology. 2020;138(May):110333. DOI: 10.1016/j.ijporl.2020.110333
Copyright (c) 2025 Angelica Diana Vita, Muhammad Hanun Mahyuddin, Dian Saraswati

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
- The journal allows the author to hold the copyright of the article without restrictions.
- The journal allows the author(s) to retain publishing rights without restrictions.
- The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
- The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.