THE RELATIONSHIP BETWEEN DURATION OF DIALYSIS AND HISTORY OF BLOOD TRANSFUSION WITH HEPATITIS C SEROPREVALENCE IN HEMODIALYSIS PATIENTS: A CROSS-SECTIONAL STUDY AT GADJAH MADA UNIVERSITY ACADEMIC HOSPITAL

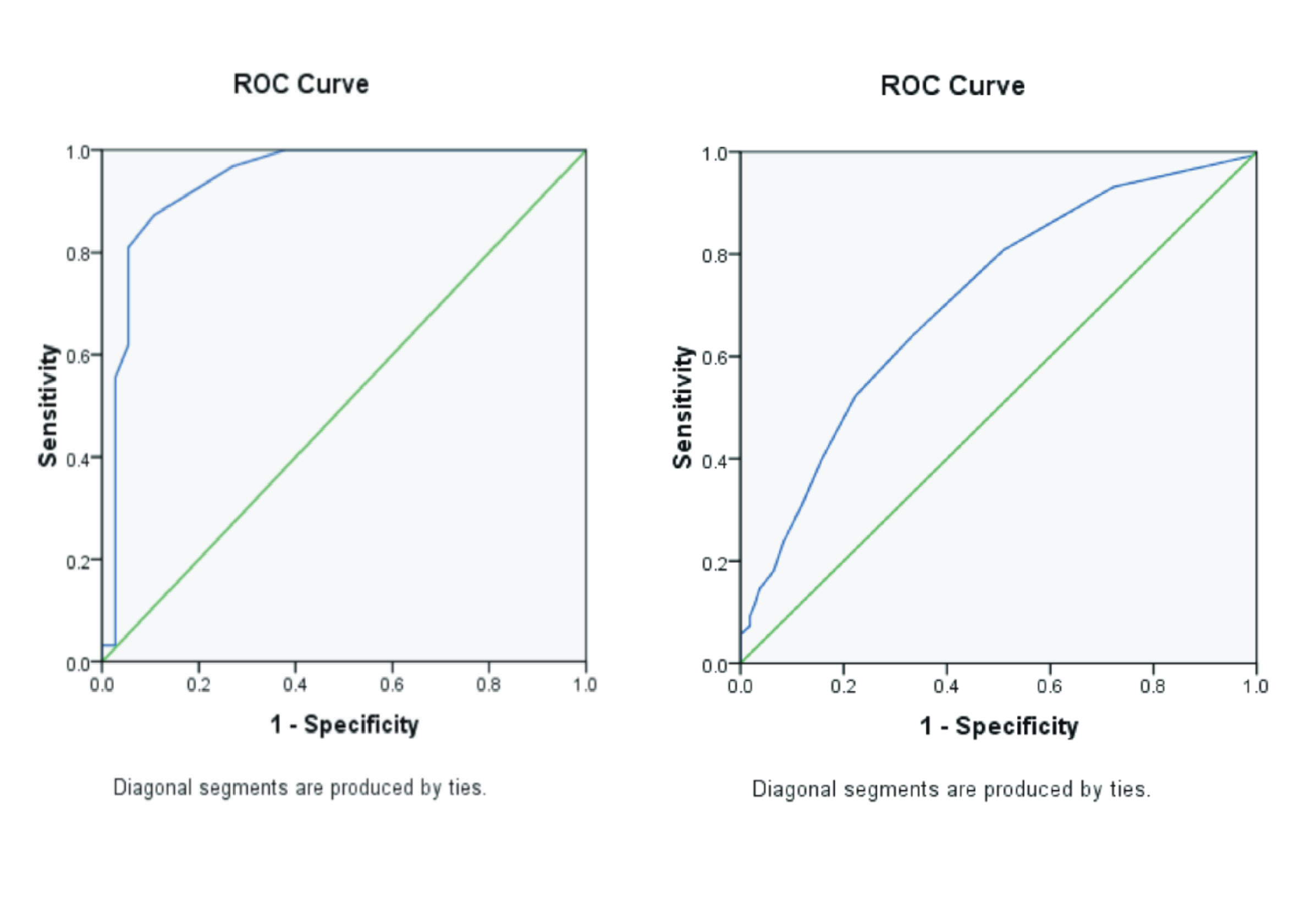
Background: Hepatitis C Virus (HCV) is an RNA virus that causes hepatitis C disease. Hemodialysis patients are a group at high risk of becoming infected with the HCV. Based on prior research, the duration of hemodialysis has been identified as an independent risk factor for HCV. Risk factors for HCV transmission in hemodialysis patients can also include blood transfusions. Purpose: This research aimed to determine the relationship between the duration of dialysis and the history of blood transfusion with HCV seroprevalence in hemodialysis patients at Gadjah Mada University Academic Hospital. Method: This research utilized a cross-sectional research design. The research data were based on secondary data from the medical records of hemodialysis patients at Gadjah Mada University Academic Hospital. Result: The results were analyzed descriptively and statistically using the Chi-square test with significance (α = 0.05). Data obtained from this research showed that the HCV seroprevalence of hemodialysis patients at Gadjah Mada University Academic Hospital is 20.5%. The test results revealed a relationship between duration of dialysis with HCV seroprevalence in hemodialysis patients is a p-value = 0.021 (p-value < α), and a relationship between history of blood transfusion with HCV seroprevalence in hemodialysis patients is a p-value = 0.024 (p-value < α). Conclusion: The results of the Chi-square test showed a relationship between duration of dialysis and history of blood transfusion with HCV seroprevalence in hemodialysis patients at Gadjah Mada University Academic Hospital.
Introduction
Hepatitis C Virus (HCV) is an RNA virus that causes hepatitis C disease. HCV that enters the body will trigger antibodies to HCV. HCV antibodies (anti-HCV) can be measured through a serological examination(Deniz & Akhan, 2023). HCV initially causes no symptoms and later develops into a chronic form, causing liver cirrhosis and liver cancer. An acute infection can result in severe liver damage and in rare cases, even lead to death(Niepmann & Gerresheim, 2020). Hemodialysis patients are a group at high risk of being infected with HCV. Hemodialysis is an invasive procedure that carries a risk of infection. Dialysis procedures, blood contamination on device surfaces, and the presence of a large number of patients undergoing dialysis in shared spaces are the causes of these risk factors. Hemodialysis patients infected with HCV can become carriers and have the potential to spread the virus in the hemodialysis environment. HCV infection within dialysis units suggests a nosocomial infection with various risk factors related to the dialysis procedure. The duration of hemodialysis was found to be an independent risk factor for HCV(Dharmesti et al., 2022). The incidence of hepatitis C in hemodialysis patients is much higher than in healthy subjects(Morishita et al., 2019).
According to the Global Hepatitis Report, people have chronic HCV infection an estimated 58 million with about 1.5 million new infections occurring per year(Organization, 2023). The prevalence of HCV in Indonesia is based on study data from the National Basic Health Research in 2014, which shows the prevalence of anti-HCV positive by 0.8 - 1% in Indonesia(Health, 2019). HCV infection is asymptomatic in its earliest stages, but up to 30% of cases progress to cirrhosis within 10 to 30 years. The probability rate of complications of liver cirrhosis to hepatocellular carcinoma associated with HCV infection is about 1 to 4% every year(Bohorquez et al., 2023). The World Health Organization (WHO) estimated that 1 in 3 people in the world have been infected by either Hepatitis B Virus (HBV) or HCV, and 1.3 million people died as a result of this disease in 2015. It has been reported that approximately 185 million of those people are infected with HCV(Jefferies et al., 2018). Chronic HCV infection is a global health burden with an estimated prevalence varying between 0.6% – 10%(Modin et al., 2019). On the seroprevalence for HCV in blood donors at UTD PMI Semarang Java Middle in 2019, the percentage of HCV reactive blood was 0.2%, namely 183 bags out of 83.074 bags(Adhyatma et al., 2020). According to a study by(Novayanti & Loesnihari, 2019), the prevalence of patients with positive anti-HCV undergoing hemodialysis was 120 patients (93.7%) out of 128 patients.
Nosocomial transmission in hemodialysis patients infected with HCV can be caused by poor hygiene of dialysis equipment. The risk factor for transmission of hepatitis infection through hemodialysis is estimated at around 10% per year. Blood transfusions can also be a risk factor for HCV transmission in hemodialysis patients, who serve as a significant medium in the transmission of HCV infection. Most cases of hepatitis infection occur after blood transfusions. About 1 per 100.000 or 0.001% of units of blood used for transfusion are at risk of HCV contamination. The average prevalence rate of HCV infection in patients who receive packed red cell or plasma transfusions is around 19%(Alhawaris, 2019). Transmission of HCV also occurs through contact with the blood or body fluids of an infected person(Mustika & Simatupang, 2020).
Research on the relationship between risk factors for duration of dialysis and history of blood transfusion with HCV seroprevalence in hemodialysis patients at the Gadjah Mada University Academic Hospital (RSA UGM) has never been conducted. Patients with an anti-HCV reactive at the RSA UGM are not isolated and do not use special machines. Hemodialysis patients with reactive anti-HCV can use a re-dialyzer. The sterilization room for repeat dialyzer used in hemodialysis patients with reactive anti-HCV and non-reactive anti-HCV is a single room, with a separate washing area. The incidence of chronic kidney failure patients undergoing hemodialysis with hepatitis C seropositivity is an indicator of the quality of the hemodialysis unit at the RSA UGM. This research aimed to determine the seroprevalence of HCV antibodies in hemodialysis patients at the RSA UGM. The purpose of this research was also to determine the relationship between risk factors for the duration of dialysis and the history of blood transfusion with seroprevalence for HCV in hemodialysis patients at the RSA UGM.
Material and Method
The data collected were analyzed through univariate and bivariate analyses. The statistical test used for this research was chi-square with a 95% confidence level. This research has been registered and obtained a research ethics permit from the Health Research Ethics Commission, Faculty of Medicine, Public Health and Nursing, Gadjah Mada University – Dr Sardjito General Hospital with registration number Ref. No.: KE/FK/0707/EC/2020 and date of approval June 30th, 2020.
The type of research used was a cross-sectional study based on secondary data from medical records of hemodialysis patients at the hemodialysis installation and the integrated clinical laboratory installation at the RSA UGM. The inclusion criteria in this research were patients undergoing hemodialysis, aged ≥18 years old, and having complete medical record data at the RSA UGM hemodialysis installation. Exclusion criteria from this research
Adhyatma, G. P., Luthfita, A., Hanjani, A., Nalaresi, A., Nurraga, G. W., Astuti, A. K. Y., Purnomo, H. D., Sofro, M. A. U. 2020. Seroprevalence Hepatitis C Reaktif pada Donor Palang Merah Indonesia Semarang, Jawa Tengah the Seroprevalence of Hepatitis C Reactive in Donors of Indonesian Red Cross Blood Bank Semarang, Central Java. Prosiding Seminar Nasional Unimus.Vol 3. Pp. 651-657.
Aditya, A., Mustofa, F. L., Hidayat, H., Firlanda, Z. R. S. 2022. Prevalensi Hepatitis C pada Donor Darah Sebelum dan pada Saat Pandemi Covid 19 di Unit Transfusi Darah Palang Merah Indonesia Provinsi Lampung Tahun 2019-2020. Malahayati Nursing Journal. Vol 4(6). Pp. 1544–1556.
Alhawaris. 2019. Hepatitis C: Epidemiology, Etiology, and Pathogenicity. Journal of Health Sciences. Vol. 2(2). Pp.139-150.
Bohorquez, M. C., Carnalla, M., Tapia, C.N., Gutiérrez, B.T. 2023. Hepatitis C Mortality Trends in Mexico from 2001 to 2017. Annals of Hepatology. Vol 28(3). Pp. 1-7.
Caragea, D.C., Mihailovoci, A.R., Streba, C.T., Schenker, M., Ungureanu, B., Caragea, I.N., Popa, R., Obleaga,C. Vere, C.C. 2018. Hepatitis C Virus Infection in Hemodialysis Patients. Current Health Sciences Journal. Vol 44 (2). Pp. 107-112.
Chizoba, O. O., Chibuogwu, A. A. 2018. Duration of Dialysis Increases Risk of Hepatitis C Virus Infections among Hemodialysis Patients in Anambra State, Nigeria. Universa Medicina. Vol 37(3). Pp. 173–180.
Dharmesti, N. W. W., Wibawa, I. D. N., Kandarini, Y. 2022. Hepatitis C Seroconversion Remains High among Patients with Regular Hemodialysis: Study of Associated Risk Factors. International Journal of Hepatology. Vol 2022. Pp. 1-8.
Deniz, M.T, Akhan, S. 2023. Hepatitis C Virus Structure and Diagnostic Methods. Intech Open Hepatitis C - Recent Advances. Pp. 1-15.
Jatikusuma, A. 2018. Identification of Positive Anti Hepatitis C Virus and Positive HCV Ribonucleic Acid in The Indonesian Red Cross, Tuban Regency, East Java. Medical Science Journal. Vol 10(2). Pp. 47–50.
Jiang, X., Chang, L., Yan, Y., Ji, H., Sun, H., Guo, F., Wang, L. 2021. A Study Based on Four Immunoassays: Hepatitis C Virus Antibody Against Different Antigens May Have Unequal Contributions to Detection. Virology Journal. Vol 18(1). Pp. 1–10.
Jefferies, M., Rauff, B., Rashid, H., Lam, T., Rafiq, S. 2018. Update on Global Epidemiology of Viral Hepatitis and Preventive Strategies. World Journal of Clinical Cases. Vol 6(13). Pp. 589–599.
Kannan, A., Biswas, L., Kumar, A., Kurian, J., Nair, A. S., Suresh, P., Sadasivan, S., Biswas, R. 2021. Improving Diagnosis of Hepatitis C Virus Infection Using Hepatitis C Core Antigen Testing in A Resource-Poor Setting. Revista Da Sociedade Brasileira de Medicina Tropical. Vol 54. Pp. 1–5.
Kerollos, K.M.N., El-Ameen, H.A., El Wahed, L.A., Azoz, N.M.A. 2020. Prevalence and Seroconversion of Hepatitis C among Hemodialysis Patients in Assiut Governorate, Egypt. The Egyptian Journal of Internal Medicine. Vol 32(1). Pp. 10–15.
Lydia, A., Larasati, A., Gani, RA., Rinaldi, I. 2019. Liver Fibrosis of Hepatitis C Virus Infection in Routine Hemodialysis Patients in Indonesia. Medical Journal of Indonesia. Vol 2. Pp. 375–379.
Martias, V. Y., Ratih, W. U., Kesehatan, P., Setya, B. 2022. Prevalensi Hepatitis C Ada Pendonor Darah di UTD PMI Kabupaten Bantul Tahun 2019-2020. Jurnal Ilmu Kesehatan Bhakti Setya Medika. Vol 7(1). Pp. 57–64.
Ministry of Health. 2019. Pedoman Nasional Pelayanan Kedokteran Tata Laksana Hepatitis C. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MENKES/681/2019
Modin, L., Arshad, A., Wilkes, B., Benselin, J., Lloyd, C., Irving, W. L., Kelly, D. A. 2019. Epidemiology and Natural History of Hepatitis C Virus Infection among Children and Young People. Journal of Hepatology. Vol 70(3). Pp. 371–378.
Morishita, A., Ogawa, C., Moriya, A., Tani, J., Yoneyama, H. 2019. Clinical Outcomes of Hepatitis C Virus Elimination Using Glecaprevir and Pibrantasvir in Hemodialysis Patients: A Multicenter Study. PubMed. Vol 50(5). Pp. 557-564.
Mustika, S., Simatupang, C. D. 2020. Prevalence of Hepatitis B and C Infection among Street Children Community in Malang City. The Indonesian Journal of Gastroenterology, Hepatology, and Digestive Endoscopy. Vol 21(1). Pp. 12–16.
Niepmann, M., Gerresheim, G. K. 2020. Hepatitis C Virus Translation Regulation. International Journal of Molecular Sciences. Vol 21(7). Pp. 1-33.
Novayanti, D., Loesnihari, R. 2019. Serokonversi Pasien Hemodialisis Reguler di RSUP. H. Adam Malik Medan pada Agustus 2016 – Juli 2017. The Journal of Medical School (JMS). Vol 52(3). Pp. 102–107.
Purwanita, P., Natsir, N. 2021. Studi Diagnostik menggunakan PCR untuk Mendeteksi Virus Hepatitis C dalam Cairan Air Mata Pasien Hemodialisis. Sriwijaya Journal of Medicine. Vol 4(1). Pp. 17–23.
Tang, Q., Chen, Z., Li, H., Zhang, L., Peng, M., Zeng, Y., Liu, X., Liu, Z., Hu, P. 2023. Molecular Epidemiology of Hepatitis C Virus Genotypes in Diferent Geographical Regions of Chinese Mainland and A Phylogenetic Analysis. Infectious Diseases of Poverty. Vol 12(66). Pp. 1-12.
WHO. World Health Organization. 2023. Hepatitis C. Available from:http: www.who.int/news-room/fact-sheets/detail/hepatitis-c (Accessed: 15 September, 2023).
Yerizel, Eti, Almurdi, Revilla, Gusti. 2018. Correlations of Viral Load Toward HCV Core Antigen and Aminotransferase in Hepatitis C Virus Genotype 1 Infection. Journal of Applied Sciences. Vol. 18(2). Pp.103-108.
Zhou, J., Wang, F. Da, Li, L. Q., Chen, E. Q. 2023. Management of In and Out of Hospital Screening for Hepatitis C. Frontiers in Public Health. Vol 10(2). Pp. 1-7.
Copyright (c) 2025 Journal of Vocational Health Studies

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- The authors agree to transfer the transfer copyright of the article to the Journal of Vocational Health Studies (JVHS) effective if and when the paper is accepted for publication.
- Legal formal aspect of journal publication accessibility refers to Creative Commons Attribution-NonCommercial-ShareAlike (CC BY-NC-SA), implies that publication can be used for non-commercial purposes in its original form.
- Every publications (printed/electronic) are open access for educational purposes, research, and library. Other that the aims mentioned above, editorial board is not responsible for copyright violation.
Journal of Vocational Health Studies is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License