THE PREVALENCE, ISOLATION, AND ANTIMICROBIAL SUSCEPTIBILITY TESTING OF ENTEROCOCCUS SPECIES FROM VARIOUS CLINICAL SAMPLES IN A TERTIARY CARE HOSPITAL

Downloads
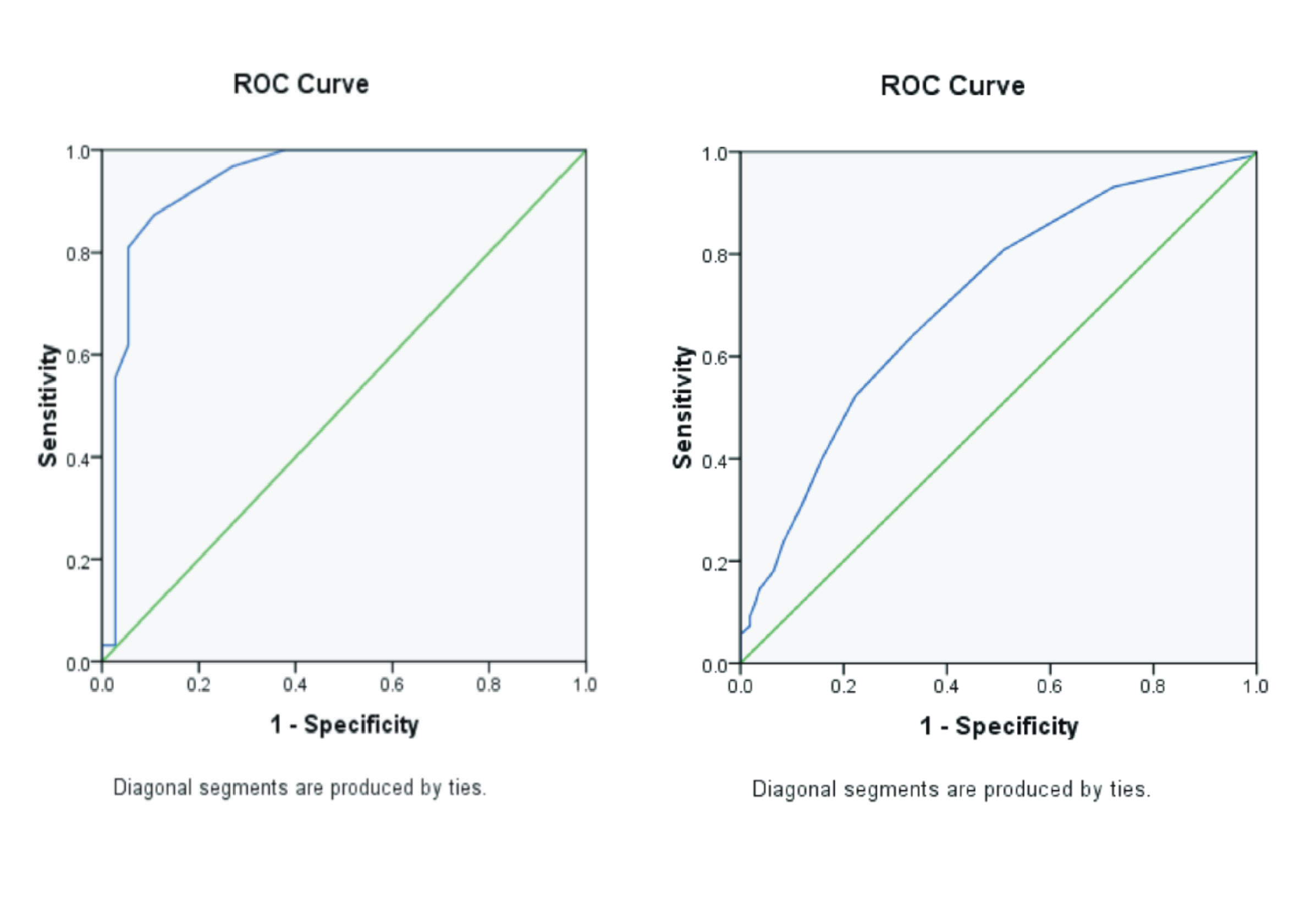
Background: Enterococcus is routinely considered a low-grade pathogen. The synergistic action of Enterococci with other bacteria increases the risk of infection. Enterococci are currently the next most common cause of healthcare-associated infections after E. coli. Greater understanding is needed regarding Enterococcus stress survival, virulence, and resistance patterns to assess the complexity of disease-causing Enterococcus. Purpose: Analyze the prevalence of Enterococcus and assess the antibiotic sensitivity pattern of Enterococcus. Method: A descriptive cross-sectional study was designed and carried out in the Department of Microbiology at Bangladesh University of Health Sciences, Dhaka, over a period of 3 months. Bacterial culture and sensitivity were the methods employed for microbiological examination. Result: A total of 558 bacterial strains were isolated, among which the growth of Enterococcus spp. was 27 (4.83%). The prevalence of Enterococcus spp. among different samples was 4.83%. The number of highly sensitive strains ranged from 66.66% to 77.77% for antibiotics, namely gentamycin, ampicillin, amoxicillin, and meropenem. Moderately high sensitivity to levofloxacin (29.62%) and low sensitivity to doxycycline (14.81%) were also analyzed. Conclusion: The study recommends that antibiotics should be used after proper laboratory procedures are undertake, and it should be selected based on antimicrobial susceptibility tests.
Afonina, I., Lim, X.N., Tan, R., Kline, K.A., 2018. Planktonic Interference and Biofilm Alliance between Aggregation Substance and Endocarditis- and Biofilm-Associated Pili in Enterococcus faecalis. J Bacteriol Vol. 200(24), Pp. e00361-18.
Ahmed, M.U., Asna, S.Z.H., Mahbub, A., 2020. Prevalence and Drug Resistance Status of Enterococcus in Tertiary Care Hospital. AIBM Vol. 16(1), Pp. 1-5.
Billington, E.O., Phang, S.H., Gregson, D.B., Pitout, J.D.D., Ross, T., Church, D.L., Laupland, K.B., Parkins, M.D., 2014. Incidence, risk factors, and outcomes for Enterococcus spp. Blood Stream Infections: A Population-Based Study. Int J Infect Dis Vol. 26, Pp. 76-82.
Coombs, G.W., Pearson, J.C., Daley, D.A., Le, T., Robinson, O.J., Gottlieb, T., Howden, B.P., Johnson, P.D.R.,Bennett, C.M., Stinear, T.P., Turnidge, J.D., Australian Group on Antimicrobial Resistance, 2014. Molecular Epidemiology of Enterococcal Bacteremia inAustralia. J Clin Microbiol Vol 52(3), Pp. 897-905.
Esmail, M.A.M., Abdulghany, H.M., Khairy, R.M., 2019. Prevalence of Multidrug-Resistant Enterococcus faecalis in Hospital-Acquired Surgical Wound Infections and Bacteremia: Concomitant Analysis of Antimicrobial Resistance Genes. Infect Dis (Auckl) Vol. 12, Pp. 1178633719882929.
Ferede, Z.T., Tullu, K.D., Derese, S.G., Yeshanew, A.G., 2018. Prevalence and Antimicrobial Susceptibility Pattern of Enterococcus Species Isolated from Different Clinical Samples at Black Lion Specialized Teaching Hospital, Addis Ababa, Ethiopia. BMC Research Notes Vol. 11(1), Pp. 793.
Ferguson, D.M., Griffith, J.F., McGee, C.D., Weisberg, S.B., Hagedorn, C., 2013. Comparison of Enterococcus Species Diversity in Marine Water and Wastewater using Enterolert and EPA Method 1600. J Environ Public Health Vol. 2013, Pp. 848049.
Govindarajan, D.K., Meghanathan, Y., Sivaramakrishnan, M., Kothandan, R., Muthusamy, A., Seviour, T.W., Kandaswamy, K., 2022.
Enterococcus Faecalis Thrives in Dual-Species Biofilm Models under Iron-Rich Conditions. Archives of Microbiology Vol. 206(710).
Horner, C., Mushtaq, S., Allen, M., Hope, R., Gerver, S., Longshaw, C., Reynolds, R., Woodford, N., Livermore, D.M., 2021. Replacement of Enterococcus faecalisby Enterococcus faecium as The PredominantEnterococcus in UK Bacteraemias. JAC AntimicrobResist Vol. 3(4), Pp. dlab185.
Hollenbeck, B.L., Rice, L.B., 2012. Intrinsic and Acquired Resistance Mechanisms in Enterococcus. Virulence Vol. 3(5), Pp. 421-433.
Hufnagel, M., Hancock, L.E., Koch, S., Theilacker, C., Gilmore, M.S., Huebner, J., 2004. Serological and Genetic Diversity of Capsular Polysaccharides in Enterococcus faecalis. Journal of Clinical Microbiology Vol. 42(6).
Huycke, M.M., Sahm, D.F., Gilmore, M.S., 1998. Multiple-Drug Resistant Enterococci: The Nature of The Problem and An Agenda for The Future. Emerg Infect Dis Vol. 4(2), Pp. 239-249.
Kim, Y., Choi, S.-I., Jeong, Y., Kang, C.-H., 2022. Evaluation of Safety and Probiotic Potential of Enterococcus faecalis MG5206 and Enterococcus faecium MG5232 Isolated from Kimchi, a Korean Fermented Cabbage. Microorganisms Vol. 10(10), Pp. 2070.
Kwit, R., ZajÄ…c, M., ÅšmiaÅ‚owska-WÄ™gliÅ„ska, A., SkarżyÅ„ska, M., Bomba, A., Lalak, A., Skrzypiec, E., Wojdat, D., Koza, W., Mikos-Wojewoda, E., Pasim, P., Skóra, M., Polak, M., WiÄ…cek, J., Wasyl, D., 2023. Prevalence of Enterococcus spp. and the Whole-Genome Characteristics of Enterococcus faecium and Enterococcus faecalis Strains Isolated from Free-Living Birds in Poland. Pathogens Vol. 12(6), Pp. 836.
Low, D.E., Keller, N., Barth, A., Jones, R.N., 2001. Clinical Prevalence, Antimicrobial Susceptibility, and Geographic Resistance Patterns of Enterococci: Results from the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clinical Infectious Diseases Vol. 32(Supp.2), Pp. S133-S145.
Marino, A., Munafò, A., Zagami, A., Ceccarelli, M., Di Mauro, R., Cantarella, G., Bernardini, R., Nunnari, G., Cacopardo, B., 2021. Ampicillin Plus Ceftriaxone Regimen against Enterococcus faecalis Endocarditis: A Literature Review. J Clin Med Vol. 10(19), Pp. 4594.
Miller, W.R., Munita, J.M., Arias, C.A., 2014. Mechanisms of Antibiotic Resistance in Enterococci. Expert Review Anti Infective Therapy Vol. 12(10), Pp.1221-1236.
Mishra, M., Sharma, D., Chauhan, D., 2022. Prevalence and Antibiotic Resistance Pattern of Isolated Enterococcus by Standard Techniques. International Journal of Health Sciences and Research Vol. 12(11), Pp. 7-11.
Moghimbeigi, A., Moghimbeygi, M., Dousti, M., Kiani, F., Sayehmiri, F., Sadeghifard, N., Nazari, A., 2018. Prevalence of Vancomycin Resistance among Isolates of Enterococci in Iran: A Systematic Review and Meta-Analysis. AHMT Vol. 9, Pp. 177-188.Monteiro Marques, J., Coelho, M., Santana, A.R., Pinto,D., Semedo-Lemsaddek, T., 2023. Dissemination of Enterococcal Genetic Lineages: A One Health Perspective. Antibiotics (Basel) Vol. 12(7), Pp. 1140.
Namikawa, H., Yamada, K., Shibata, W., Fujimoto, H., Takizawa, E., Niki, Makoto, Nakaie, K., Nakamura, Y., Oinuma, K.-I., Niki, Mamiko, Takemoto, Y., Kaneko, Y., Shuto, T., Kakeya, H., 2017. Clinical Characteristics and Low Susceptibility to Daptomycin in Enterococcus faecium Bacteremia. The Tohoku Journal of Experimental Medicin Vol. 243(3), Pp. 211-218.
Paul, M., Nirwan, P.S., Srivastava, P., 2017. Isolation of Enterococcus from Various Clinical Samples and Their Antimicrobial Susceptibility Pattern in a Tertiary Care Hospital. Int.J.Curr.Microbiol.App.Sci Vol. 6(2), Pp. 1326-1332.
Ramos, S., Silva, V., Dapkevicius, M. de L.E., Igrejas, G., Poeta, P., 2020. Enterococci, from Harmless Bacteria to a Pathogen. Microorganisms Vol.8(8), Pp. 1118.
Sabouni, F., Pourakbari, B., Aghdam, M.K., Mahmoudi, S., Ashtiani, M.T.H., Movahedi, Z., Alyari, A.E., Sadeghi, R.H., MAMISHI, S., 2012. High Frequency of Vancomycin-Resistant Enterococcus Faecalis in an Iranian Referral Children Medical Hospital. Maedica (Bucur) Vol. 7(3), Pp. 201-204.
Siddig, L., Hamid, O., Elhadi, N., Bayoumi, M., 2022. Prevalence and Antimicrobial Profile of Colonized Enterococcus Spe-cies Isolated from Hospitalized and Non-hospitalized Patients. American Journal of Infectious Diseases and Microbiolo-gy Vol. 10(4), Pp. 119-123.
Seputiene, V., Bogdaite, A., Ruzauskas, M., Suziedeliene, E., 2012. Antibiotic Resistance Genes and Virulence Factors in Enterococcus faecium and Enterococcus faecalis from Diseased Farm Animals: Pigs, Cattle and Poultry. Pol J Vet Sci Vol.15(3), Pp. 431-438.
Spengler, G., Martins, A., Schelz, Z., Rodrigues, L., Aagaard, L., Martins, M., Costa, S.S., Couto, I., Viveiros, M., Fanning, S., Kristiansen, J.E., Molnar, J., Amaral, L., 2009. Characterization of Intrinsic Efflux Activity of Enterococcus Faecalis ATCC29212 by A Semi-Automated Ethidium Bromide Method. In Vivo Vol. 23(1), Pp. 81-87.
Sreeja, S., Babu P R, S., Prathab, A.G., 2012. The Prevalence and The Characterization of The Enterococcus Species from Various Clinical Samples in A Tertiary Care Hospital. J Clin Diagn Res Vol. 6(9), Pp. 1486-1488.
Tedim, A.P., Ruiz-Garbajosa, P., Corander, J., Rodríguez, C.M., Cantón, R., Willems, R.J., Baquero, F., Coque,T.M., 2015. Population Biology of IntestinalEnterococcus Isolates From Hospitalized andNonhospitalized Individuals in Different AgeGroups. Appl Environ Microbiol Vol. 81(5), Pp. 1820-1831.
Tuncay, R.M., Sancak, Y.C., 2022. The Prevalence of Enterococcus spp., Resistance Profiles, the Presence of the VanA and VanB Resistance Genes in Chicken Meats. Kocatepe Veterinary Journal Vol. 15(4), Pp. 381-389.
Yadav, G., Thakuria, B., Madan, M., Agwan, V., Pandey, A., 2017. Linezolid and Vancomycin Resistant Enterococci: A Therapeutic Problem - PubMed. Journal of Clinical And Diagnostic Research: JCDR Vol. 11(8), Pp. GC07-GC11.
Yoshino, Y., 2023. Enterococcus casseliflavus Infection: A Review of Clinical Features and Treatment. Infect Drug Resist Vol. 16, 363–368.
Zaheer, R., Cook, S.R., Barbieri, R., Goji, N., Cameron, A., Petkau, A., Polo, R.O., Tymensen, L., Stamm, C., Song, J., Hannon, S., Jones, T., Church, D., Booker, C.W., Amoako, K., Van Domselaar, G., Read, R.R.,McAllister, T.A., 2020. Surveillance of Enterococcus spp. Reveals Distinct Species and AntimicrobialResistance Diversity Across A One-HealthContinuum. Sci Rep Vol.10(1), Pp. 3937
Copyright (c) 2024 Journal of Vocational Health Studies

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- The authors agree to transfer the transfer copyright of the article to the Journal of Vocational Health Studies (JVHS) effective if and when the paper is accepted for publication.
- Legal formal aspect of journal publication accessibility refers to Creative Commons Attribution-NonCommercial-ShareAlike (CC BY-NC-SA), implies that publication can be used for non-commercial purposes in its original form.
- Every publications (printed/electronic) are open access for educational purposes, research, and library. Other that the aims mentioned above, editorial board is not responsible for copyright violation.
Journal of Vocational Health Studies is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License