CORRELATION BETWEEN THROMBOCYTOPENIA DEGREE AND PARASITE DENSITY IN CONFIRMED CASES OF Plasmodium falciparum AND Plasmodium vivax MALARIA

Background: Thrombocytopenia, a condition characterized by a low platelet count, is the most prevalent hematological abnormality observed in acute malaria patients. Malaria remains a major global public health problem, with more than 200 million clinical cases reported annually. Purpose: This study aimed to investigate the correlation between the degree of thrombocytopenia and the parasite density in confirmed cases of Plasmodium falciparum and Plasmodium vivax. Method: This research was a descriptive observational study using a cross-sectional design. Clinical hematological examinations and peripheral blood smear preparations were performed on malaria patients, followed by analysis of platelet count, hemoglobin levels, and leukocyte count. Result: Thrombocytopenia, commonly found in acute malaria, was observed in 63.4% of cases, underscoring its key role as a diagnostic biomarker. This study showed significant association between hemoglobin levels and thrombocytopenia severity (p-value < 0.05), whereas leukocyte counts did not show a significant association with thrombocytopenia severity (p-value > 0.05). The degree of thrombocytopenia differed between the two types of malaria, assisting the differentiation of infections. Anemia, another detailed hematological indicator, frequently found in P. falciparum cases. Conclusion: Understanding hematological indicator as key-role of malaria diagnosis is vital for accurate diagnosis and effective management of malaria, especially in endemic regions. Continued research and routine hematological surveillance are crucial to improving malaria control and treatment outcomes.
Introduction
Malaria is an infectious disease associated with varying degrees of hematological complications with anemia and thrombocytopenia being the most common manifestations(Sharma et al., 2017). According to the World Health Organization (WHO), approximately 40% of the global population is at risk of malaria infection. The annual incidence of malaria reported among 300 to 500 million cases, reached two million deaths each year(Arif et al., 2016). In Indonesia, there are five species of malaria exist,Plasmodium falciparum(P. falciparum),Plasmodium vivax(P. vivax),P. malariae,P. ovale, andP. knowlesi(Zein et al., 2017).
Early clinical detection of malaria is critical for its successful treatment. Diagnosis is typically performed using light microscopy to examine thick and thin blood smears, which remains the most reliable and widely applicable method for detecting malaria. The severity of malaria is associated to the parasitemia degree, with high levels of parasitemia resulting in severe malaria(Antwi-Baffour et al., 2023). Severe malaria is defined by the presence of asexual stage of malaria parasites, accompanied by serious symptoms or complications of malaria(Naing & Whittaker, 2018). SevereP. falciparummalaria is obvious shown on clinical manifestations, including decreased consciousness, multiple convulsions, acute respiratory distress, circulatory collapse or shock, acute kidney injury, prostration, clinical jaundice, and abnormal bleeding. A study conducted in Bangkok showed lower platelet count in cases of severe malaria compared to malaria without serious complications(Mon et al., 2022).
According to the latest WHO guidelines, hematological indices, including thrombocytopenia, are not considered criteria for defining severe malaria, however their clinical significance is widely recognized(Teparrukkul et al., 2019). A retrospective study involving 614 patients revealed that individuals with thrombocytopenia were more likely to develop Multi-Organ Dysfunction (MOD) and had an increased risk of mortality compared to malaria patients with normal platelet counts(Gill et al., 2013).
Thrombocytopenia is a known complication of malaria caused byP. falciparuminfection. However, recent studies have shown thatP. vivaxshow similar levels of severity(Bayleyegn et al., 2021). Hematological indices of malaria patients have reveal thrombocytopenia, which has been linked to excessive platelet sequestration and a shortened platelet lifespan(Lestari, 2019);(Muley et al., 2014). The proposed mechanisms leading to thrombocytopenia include coagulation disturbances, splenomegaly, bone marrow alterations, antibody-mediated platelet destruction, oxidative stress, and the role of platelets as cofactors in triggering severe malaria(Kumar et al., 2022);(Muley et al., 2014);(Natalia, 2014).
This study aimed to assess the importance of thrombocytopenia and its potential role as an early diagnostic marker for malaria. The presence of thrombocytopenia can serve as a noticeable clinical indicator of malaria symptoms. In addition to, this study sought to establish a correlation between the presence of thrombocytopenia and the type of malaria in regions where malaria is endemic in Indonesia.
Material and Method
This descriptive observational study employed a cross-sectional design. The research involved clinical hematological examinations and peripheral blood smears analyses of malaria patients visited a laboratory in Jayapura, which were then analyzed for platelet count, hemoglobin levels, and leukocyte count. Blood samples were collected from people with malaria who visited healthcare service units. The blood samples were stored in ethylenediaminetetraacetic acid (EDTA) tubes and used to prepare thin and thick blood films for giemsa staining and microscopic identification of malaria parasites and species. In this study, individuals with malaria were diagnosed through blood smear examination, and automated hematology analyzer used to assess hematological indicators. Trained medical laboratory scientists collected the blood samples, and blood counts were conducted using the Sysmex XP-100 hematology analyzer.
To discover the density of malaria parasites, a blood technician independently counted the asexual stagePlasmodiumparasites on slides, specifically counting 200 White Blood Cells (WBCs) in thick blood films from each malaria case. The counts from two independent technician were then averaged, and this mean value was used to calculate the parasite density. The number of parasites per microliter (μL) of blood was then determined using the following Formula (1).
\( \documentclass{article} \usepackage{amsmath} \begin{document} \displaystyle \text{Parasite}/\mu\text{L} = \frac{\text{parasite counted}}{200} \times \text{total WBC count} \quad \text{.... (1)} \end{document} \)
Platelet counts were determined by directly measuring platelet pulses and was expressed as thousands of platelets per microliter of whole blood. Thrombocytopenia was defined as a platelet count of less than 150.000/μL. Patients were categorized into three subgroups based on their platelet counts. Thrombocytopenia was considered severe if the platelet count was less than 50.000/μL, moderate if it ranged from 50.000 to 100.000/μL, and mild if it fell between 100.000 and 150.000/μL(Kumar et al., 2022).
Malaria parasite density was determined using the aforementioned formula and was categorized as mild, moderate, or severe parasitemia. Blood samples with 5 – 10.000 parasites/μL could be considered as low parasitemia corresponding to mild malaria, and those with 10.000 –100.000 parasites/μL were categorized as intermediate parasitemia indicating moderate malaria, whilst parasitemia above 100.000 parasites/μL was classified as hyper parasitemia and described as severe malaria which may lead to death(Wilairatana et al., 2013).
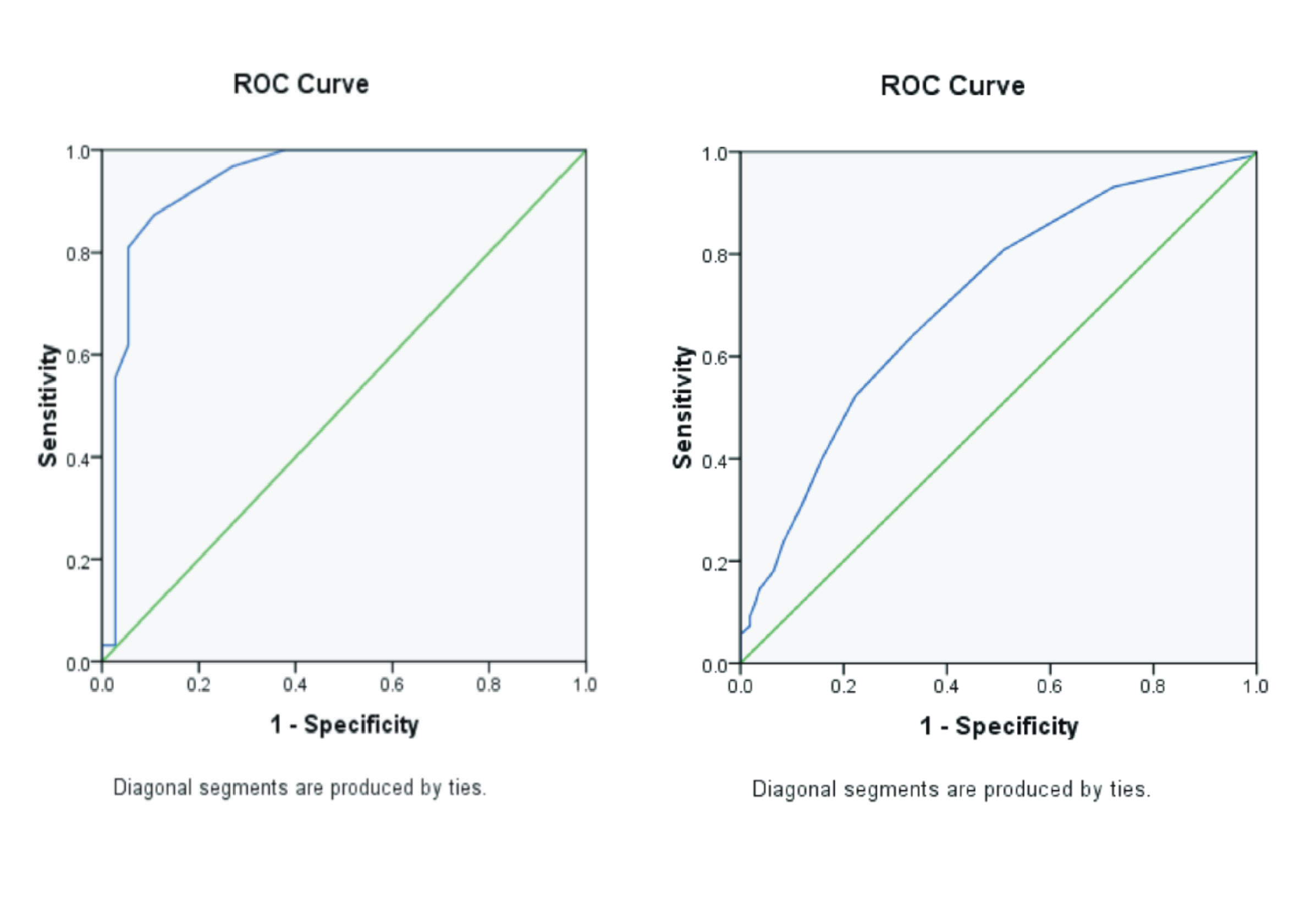
Thrombocytopenia and parasite density were treated as ordinal variables. To evaluate the correlation between them, the Spearman’s rank correlation test was used. A p-value of less than 0.05 was considered statistically significant.
Result
A total of 41 eligible patients were enrolled and randomly assigned in the study, with their characteristics summarized inTable 1. Among
Antwi-Baffour, S., Mensah, B.T., Johnson, G., Armah, D.N.O., Ali-Mustapha, S., Annison, L., 2023.Haematological Parameters and Their Correlationwith The Degree of Malaria Parasitaemia amongOutpatients Attending A Polyclinic. Malaria Journal Vol. 22(1), Pp. 281.
Arif, M., Jelia, S., Meena, S.R., Meena, S., Jain, P., Ajmera, D., Jatav, V.S., Agarwal, V., 2016. A Study of Thrombocytopenia in Malaria and Its Prognostic Significance. International Journal of Research in Medical Sciences Vol. 4(6), Pp. 2373-2378.
Awoke, N., Arota, A., 2019. Profiles of Hematological Parameters in Plasmodium Falciparum and Plasmodium Vivax Malaria Patients Attending Tercha General Hospital, Dawuro Zone, South Ethiopia. Infection and Drug Resistance Vol. 12, Pp. 521-527.
Barada, B., Mehta, A.D., Salvi, J., 2023. Evaluation of Incidence of Thrombocytopenia in Malarial Patients at A Tertiary Hospital. International Journal of Life Sciences Vol. 12(2), Pp. 1556-1558.
Bayleyegn, B., Asrie, F., Yalew, A., Woldu, B., 2021. Role of Platelet Indices as a Potential Marker for Malaria Severity. Journal of Parasitology Research Vol. 2021, Pp. 5531091.
Costa, A.G., Chaves, Y.O., Teixeira-Carvalho, A., Ramasawmy, R., Antonelli, L.R.V., Barbosa, L., Balieiro, A., Monteiro, W.M., Mourão, M.P., Lacerda, M.V.G., Martins-Filho, O.A., Costa, F.T.M., Malheiro,A., Nogueira, P.A., 2020. Increased Platelet Distribution Width and Reduced Il-2 And Il-12 Are Associated with Thrombocytopenia in Plasmodium Vivax Malaria. Memorias do Instituto Oswaldo Cruz Vol. 115, Pp. e200080.
Gill, M., Bhat, S., Dhir, G., Makkar, M., Kaur, T., 2013. Thrombocytopenia in Malaria and Its Correlation with Different Types of Malaria. Annals of Tropical Medicine and Public Health Vol. 6(2), Pp. 197.
Gupta, P., Guddattu, V., Saravu, K., 2019. Characterization of Platelet Count and Platelet Indices and Their Potential Role to Predict Severity in Malaria. Pathogens and Global Health Vol. 113(2), Pp. 86-93.
Haroon, A., Zameer, H., Naz, A., Afzal, S., Ammar, T., Zafar, I., 2021. Deranged Hematological Profile in Patients Presenting with Malarial Parasitaemia. International Journal of Community Medicine and Public Health Vol. 8(12), Pp. 1-5.
Khalid, M., Iqbal, K., Nadeem, M., Khan, K., Kousar, A., Rao, S., Abrar, M., Abbas, F., 2022. Frequency of Thrombocytopenia in Malaria Patient at Tertiary Care Hospital. Pakistan Journal of Medical & Health Sciences Vol. 16(2), Pp. 362-364.
Krishna, P., Chalamalasetty, M., 2023. Thrombocytopenia in Malaria and Its Diagnostic Significance: A Prospective Study. Journal of Clinical and Scientific Research Vol. 12(Suppl 1), Pp. S1-S4.
Kumar, M., Kumar, A., Panwar, P., Kant, R., 2022. Correlation of Presence and Severity of Thrombocytopenia with Types and Severity of Malaria: A Study from Tertiary Care Center of North India. Journal of Family Medicine and Primary Care Vol. 11(7), Pp. 3929-3933.
Lestari, A.I., 2019. Different amount of Thrombocytes on Blood Storage for 24 Hours in Room and Refrigerator Vol. 3(2), Pp. 59-62.
Mon, N.T.S., Tangpukdee, N., Charunwatthana, P., Boonnak, K., Krudsood, S., Kano, S., Wilairatana, P., Leowattana, W., 2022. Mimicking Platelet Indices in Patients with Malaria and Dengue Hemorrhagic Fever: Characteristics and Clinical Applications. Tropical Medicine and Health Vol. 50(1), Pp. 76.
Muflikhah, N., Nuraini, F., 2023. An Increase of Human Immunodeficiency Virus Infection amongs Blood Donor during COVID-19 Pandemic. International Journal of Public Health Science (IJPHS) Vol. 12(3), Pp. 1270.
Muley, A., Lakhani, J., Bhirud, S., Patel, A., 2014. Thrombocytopenia in Plasmodium Vivax Malaria: How Significant? Journal of Tropical Medicine Vol. 2014, Pp. 567469.
Naing, C., Whittaker, M.A., 2018. Severe Thrombocytopaenia in Patients with Vivax Malaria Compared to Falciparum Malaria: A Systematic Review and Meta-Analysis. Infectious Diseases of Poverty Vol. 7(1), Pp. 10.
Natalia, D., 2014. Peranan Trombosit dalam Patogenesis Malaria. Majalah Kedokteran Andalas Vol. 37(3), Pp. 219-225.
Punnath, K., Dayanand, K.K., Chandrashekar, V.N., Achur, R.N., Kakkilaya, S.B., Ghosh, S.K., Kumari, S.N., Gowda, D.C., 2019. Association between InflammatoryCytokine Levels and Thrombocytopenia duringPlasmodium Falciparum and P. Vivax Infections in South-Western Coastal Region of India. Malaria Res earch and Treatement Vol. 2019, Pp. 4296523.
Sharma, M., Srivastava, K., Mitchell, W., 2017. Malaria and Thrombopoiesis: A Possible Mechanism for The Malarial Thrombocytopenia. Journal of Immunology, Infection & Inflammatory Diseases. Vol. 2(3), Pp. 014.
Suryadi, D., Madonna, V., Sihotang, F., Siagian, L., 2021. Relationship Between Types of Plasmodium Falciparum and Plasmodium Vivax with The Degree of Thrombocytopenia in Malaria Patients At RSUD Ratu Aji Putri Botung Penajam Paser Utara. Jurnal Ilmu Kesehatan Vol. 9(1), Pp. 62-71.
Tabassum, A., Iqbal, M., 2021. Hematological Profile in Smear Positive Malaria Cases: A Cross-Sectional Study. Annals of the Romanian Society for Cell Biology Vol. 25(4), Pp. 2297-2309.
Teparrukkul, P., Hantrakun, V., Imwong, M., Teerawattanasook, N., Wongsuvan, G., Day, N.P., Dondorp, A.M., West, T.E., Limmathurotsakul, D., 2019. Utility of qSOFA and Modified SOFA in Severe Malaria Presenting as Sepsis. PLoS One Vol. 14(10), Pp. e0223457.
Wilairatana, P., Tangpukdee, N., Krudsood, S., 2013. Definition of Hyperparasitemia in Severe Falciparum Malaria Should be Updated. Asian Pasific Journal of Tropical Biomedicine Vol. 3(7), Pp. 586.
Zein, U., Habib, H., Lim, H., Fitri, L., 2017. A New Endemic Area of Ovale Malaria in Indonesia: A Case Report from Sumatra Utara. Asian Pacific Journal of Tropical Disease Vol. 7(7), Pp. 440-441
Copyright (c) 2025 Journal of Vocational Health Studies

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- The authors agree to transfer the transfer copyright of the article to the Journal of Vocational Health Studies (JVHS) effective if and when the paper is accepted for publication.
- Legal formal aspect of journal publication accessibility refers to Creative Commons Attribution-NonCommercial-ShareAlike (CC BY-NC-SA), implies that publication can be used for non-commercial purposes in its original form.
- Every publications (printed/electronic) are open access for educational purposes, research, and library. Other that the aims mentioned above, editorial board is not responsible for copyright violation.
Journal of Vocational Health Studies is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License