A Systematic Review of Endocrine Therapy for Improved Reproductive and Metabolic Outcomes in PCOS Women
Downloads
Introduction: Polycystic ovarian syndrome (PCOS) is characterized by infrequent or absent ovulation as well as elevated levels of androgens and insulin (hyperinsulinaemia). The purpose of this study was to determine the efficacy of endocrine treatment in improving reproductive and metabolic outcomes in women with PCOS.
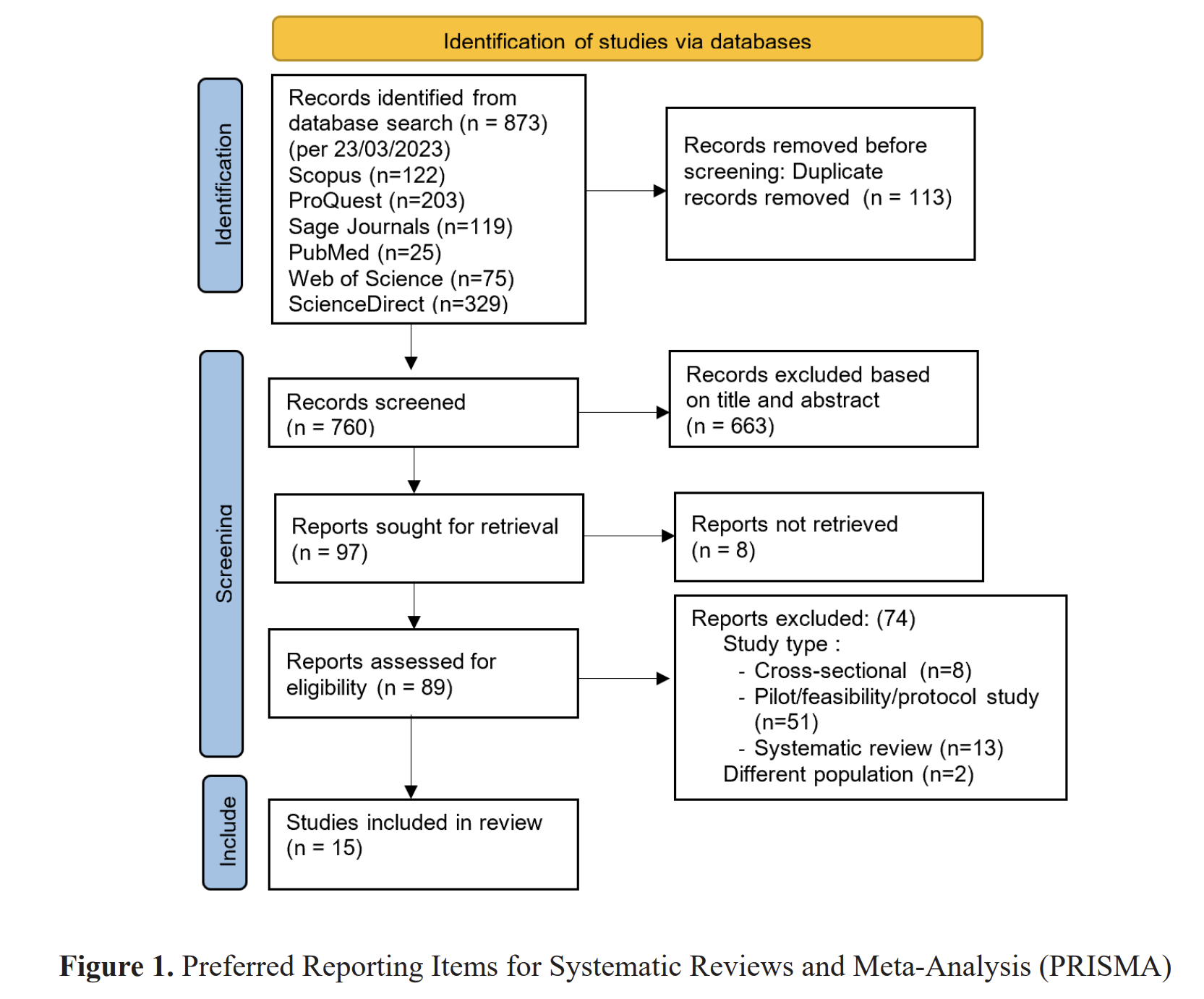
Methods: We searched the following databases from inception to Maret 2020: PubMed, Proquest, ScienceDirect, Scopus and CINAHL. We investigated at metformin, clomiphene citrate, metformin plus clomiphene citrate, D-chiro-inositol, statins, and resveratrol as treatments. We compared them to each other, as well as to a placebo or no therapy. The quality of the evidence ranged from extremely low to moderate. The risks of bias (poor reporting of technique and inadequate outcome data), imprecision, and inconsistency were the limitations.
Results: Although the evidence quality was low, our latest evaluation indicated that metformin alone may be superior to placebo for live birth. Data for live birth were equivocal when metformin was compared to clomiphene citrate, and our conclusions were hampered by a paucity of evidence. Body mass index (BMI) varies in the results, emphasizing the need of stratifying data by BMI.
Conclusion: Clinical pregnancy and ovulation improvements demonstrate that clomiphene citrate is still preferred to metformin for ovulation induction in obese women with PCOS.Abdalla, M. A., Deshmukh, H., Atkin, S., & Sathyapalan, T. (2020). A review of therapeutic options for managing the metabolic aspects of polycystic ovary syndrome. Therapeutic Advances in Endocrinology and Metabolism, 11, 1–19. https://doi.org/10.1177/2042018820938305
Almalki, H. H., Alshibani, T. M., Alhifany, A. A., & Almohammed, O. A. (2020). Comparative efficacy of statins, metformin, spironolactone and combined oral contraceptives in reducing testosterone levels in women with polycystic ovary syndrome: A network meta-analysis of randomized clinical trials. BMC Women's Health, 20(1), 1–6. https://doi.org/10.1186/s12905-020-00919-5
Altinok, M. L., Ravn, P., Andersen, M., & Glintborg, D. (2018). Effect of 12-month treatment with metformin and/or oral contraceptives on health-related quality of life in polycystic ovary syndrome. Gynecological Endocrinology, 34(10), 859–863. https://doi.org/10.1080/09513590.2018.1460343
Balen, A. H., Morley, L. C., Misso, M., Franks, S., Legro, R. S., Wijeyaratne, C. N., Stener-Victorin, E., Fauser, B. C. J. M., Norman, R. J., & Teede, H. (2016). The management of anovulatory infertility in women with polycystic ovary syndrome: An analysis of the evidence to support the development of global WHO guidance. Human Reproduction Update, 22(6), 687–708. https://doi.org/10.1093/humupd/dmw025
Banaszewska, B., Pawelczyk, L., & Spaczynski, R. (2019). Current and future aspects of several adjunctive treatment strategies in polycystic ovary syndrome. Reproductive Biology, 19(4), 309–315. https://doi.org/10.1016/j.repbio.2019.09.006
Brennan, L., Teede, H., Skouteris, H., Linardon, J., Hill, B., & Moran, L. (2017). Lifestyle and Behavioral Management of Polycystic Ovary Syndrome. Journal of Women's Health. https://doi.org/10.1089/jwh.2016.5792
Charifson, M. A., & Trumble, B. C. (2019). Evolutionary origins of polycystic ovary syndrome: An environmental mismatch disorder. Evolution, Medicine and Public Health, 2019(1), 50–63. https://doi.org/10.1093/emph/eoz011
Costello, M. F., Misso, M. L., Balen, A., Boyle, J., Devoto, L., Garad, R. M., Hart, R., Johnson, L., Jordan, C., Legro, R. S., Norman, R. J., Moran, L., Mocanu, E., Qiao, J., Rodgers, R. J., Rombauts, L., Tassone, E. C., Thangaratinam, S., Vanky, E., & Teede, H. J. (2019). A brief update on the evidence supporting the treatment of infertility in polycystic ovary syndrome. Australian and New Zealand Journal of Obstetrics and Gynaecology, 59(6), 867–873. https://doi.org/10.1111/ajo.13051
Cozzolino, M., Vitagliano, A., Pellegrini, L., Chiurazzi, M., Andriasani, A., Ambrosini, G., & Garrido, N. (2020). Therapy with probiotics and synbiotics for polycystic ovarian syndrome: a systematic review and meta-analysis. European Journal of Nutrition, 0123456789. https://doi.org/10.1007/s00394-020-02233-0
De Diego, M. V., Gómez-Pardo, O., Groar, J. K., López-Escobar, A., Martín-Estal, I., Castilla-Cortázar, I., & Rodríguez-Zambrano, M. Á. (2020). Metabolic impact of current therapeutic strategies in Polycystic Ovary Syndrome: a preliminary study. Archives of Gynecology and Obstetrics, 0123456789. https://doi.org/10.1007/s00404-020-05696-y
Della Corte, L., Foreste, V., Barra, F., Gustavino, C., Alessandri, F., Centurioni, M. G., Ferrero, S., Bifulco, G., & Giampaolino, P. (2020). Current and experimental drug therapy for the treatment of polycystic ovarian syndrome. Expert Opinion on Investigational Drugs, 0(0). https://doi.org/10.1080/13543784.2020.1781815
Dokras, A., Playford, M., Kris-Etherton, P. M., Kunselman, A. R., Stetter, C. M., Williams, N. I., Gnatuk, C. L., Estes, S. J., Sarwer, D. B., Allison, K. C., Coutifaris, C., Mehta, N., & Legro, R. S. (2017). Impact of hormonal contraception and weight loss on high-density lipoprotein cholesterol efflux and lipoprotein particles in women with polycystic ovary syndrome. Clinical Endocrinology, 86(5), 739–746. https://doi.org/10.1111/cen.13310
Jeanes, Y. M., & Reeves, S. (2017). Metabolic consequences of obesity and insulin resistance in polycystic ovary syndrome: Diagnostic and methodological challenges. In Nutrition Research Reviews. https://doi.org/10.1017/S0954422416000287
Jensterle, M., Kravos, N. A., Ferjan, S., Goricar, K., Dolzan, V., & Janez, A. (2020). Long-term efficacy of metformin in overweight-obese PCOS: Longitudinal follow-up of retrospective cohort. Endocrine Connections, 9(1), 44–54. https://doi.org/10.1530/EC-19-0449
Jin, P., & Xie, Y. (2018). Treatment strategies for women with polycystic ovary syndrome. Gynecological Endocrinology, 34(4), 272–277. https://doi.org/10.1080/09513590.2017.1395841
Kim, C. H., Chon, S. J., & Lee, S. H. (2020). Effects of lifestyle modification in polycystic ovary syndrome compared to metformin only or metformin addition: A systematic review and meta-analysis. Scientific Reports, 10(1), 1–14. https://doi.org/10.1038/s41598-020-64776-w
Li, Y., Tan, J., Wang, Q., Duan, C., Hu, Y., & Huang, W. (2020). Comparing the individual effects of metformin and rosiglitazone and their combination in obese women with polycystic ovary syndrome: a randomized controlled trial. Fertility and Sterility, 113(1), 197–204. https://doi.org/10.1016/j.fertnstert.2019.09.011
Macut, D., Bjekić-Macut, J., Rahelić, D., & Doknić, M. (2017). Insulin and the polycystic ovary syndrome. Diabetes Research and Clinical Practice, 130, 163–170. https://doi.org/10.1016/j.diabres.2017.06.011
Macut, D., Božić-Antić, I., Bjekić-Macut, J., & Tziomalos, K. (2017). Management of endocrine disease: Polycystic ovary syndrome and nonalcoholic fatty liver disease. European Journal of Endocrinology, 177(3), R145–R158. https://doi.org/10.1530/EJE-16-1063
Moradi, F., Ghadiri-Anari, A., Dehghani, A., Vaziri, S. R., & Enjezab, B. (2020). The effectiveness of counseling based on acceptance and commitment therapy on body image and self-esteem in polycystic ovary syndrome: An RCT. International Journal of Reproductive BioMedicine, 18(4), 243–252. https://doi.org/10.18502/ijrm.v13i4.6887
Moran, L. J., Tassone, E. C., Boyle, J., Brennan, L., Harrison, C. L., Hirschberg, A. L., Lim, S., Marsh, K., Misso, M. L., Redman, L., Thondan, M., Wijeyaratne, C., Garad, R., Stepto, N. K., & Teede, H. J. (2020). Evidence summaries and recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome: Lifestyle management. Obesity Reviews, 21(10), 1–15. https://doi.org/10.1111/obr.13046
Morgante, G., Massaro, M. G., Scolaro, V., Cappelli, V., Luddi, A., Troí¬a, L., & De Leo, V. (2020). Metformin doses and body mass index: clinical outcomes in insulin resistant polycystic ovary syndrome women. European Review for Medical and Pharmacological Sciences, 24(15), 8136–8142. https://doi.org/10.26355/eurrev_202008_22500
Morley, L. C., Tang, T., Yasmin, E., Norman, R. J., & Balen, A. H. (2017). Insulin-sensitising drugs (metformin, rosiglitazone, pioglitazone, D-chiro-inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility. Cochrane Database of Systematic Reviews, 2017(11). https://doi.org/10.1002/14651858.CD003053.pub6
Podfigurna, A., Meczekalski, B., Petraglia, F., & Luisi, S. (2020). Clinical, hormonal and metabolic parameters in women with PCOS with different combined oral contraceptives (containing chlormadinone acetate versus drospirenone). Journal of Endocrinological Investigation, 43(4), 483–492. https://doi.org/10.1007/s40618-019-01133-3
Sharpe, A., Morley, L. C., Tang, T., Norman, R. J., & Balen, A. H. (2019). Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews, 2019(12). https://doi.org/10.1002/14651858.CD013505
Wang, A., Mo, T., Li, Q., Shen, C., & Liu, M. (2019). The effectiveness of metformin, oral contraceptives, and lifestyle modification in improving the metabolism of overweight women with polycystic ovary syndrome: a network meta-analysis. Endocrine, 64(2), 220–232. https://doi.org/10.1007/s12020-019-01860-w
Wang, Q. Y., Song, Y., Huang, W., Xiao, L., Wang, Q. S., & Feng, G. M. (2016). Comparison of drospirenone-with cyproterone acetate-containing oral contraceptives, combined with metformin and lifestyle modifications in women with polycystic ovary syndrome and metabolic disorders: A prospective randomized control trial. Chinese Medical Journal, 129(8), 883–890. https://doi.org/10.4103/0366-6999.179783
Zeng, X., Xie, Y. jie, Liu, Y. ting, Long, S. lian, & Mo, Z. cheng. (2020). Polycystic ovarian syndrome: Correlation between hyperandrogenism, insulin resistance and obesity. Clinica Chimica Acta, 502, 214–221. https://doi.org/10.1016/j.cca.2019.11.003
Zhang, B., Zhang, B., Zhang, B., Zhang, B., Zhou, W., Zhou, W., Zhou, W., Zhou, W., Shi, Y., Shi, Y., Shi, Y., Shi, Y., Zhang, J., Cui, L., Cui, L., Cui, L., Cui, L., Chen, Z. J., Chen, Z. J., ... Chen, Z. J. (2020). Lifestyle and environmental contributions to ovulatory dysfunction in women of polycystic ovary syndrome. BMC Endocrine Disorders, 20(1), 1–7. https://doi.org/10.1186/s12902-020-0497-6
Zhang, J., Si, Q., & Li, J. (2017). Therapeutic effects of metformin and clomiphene in combination with lifestyle intervention on infertility in women with obese polycystic ovary syndrome. Pakistan Journal of Medical Sciences, 33(1), 8–12. https://doi.org/10.12669/pjms.331.11764
Copyright (c) 2021 NUR AINI LUTFI RAHMAWATI

This work is licensed under a Creative Commons Attribution 4.0 International License.
1. The journal allows the author to hold the copyright of the article without restrictions.
2. The journal allows the author(s) to retain publishing rights without restrictions.
3. The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution (CC BY).