PROFILE OF HIV/AIDS PATIENTS COINFECTED WITH TUBERCULOSIS IN IBNU SINA DISTRICT HOSPITAL, GRESIK,EAST JAVA, INDONESIA
Downloads
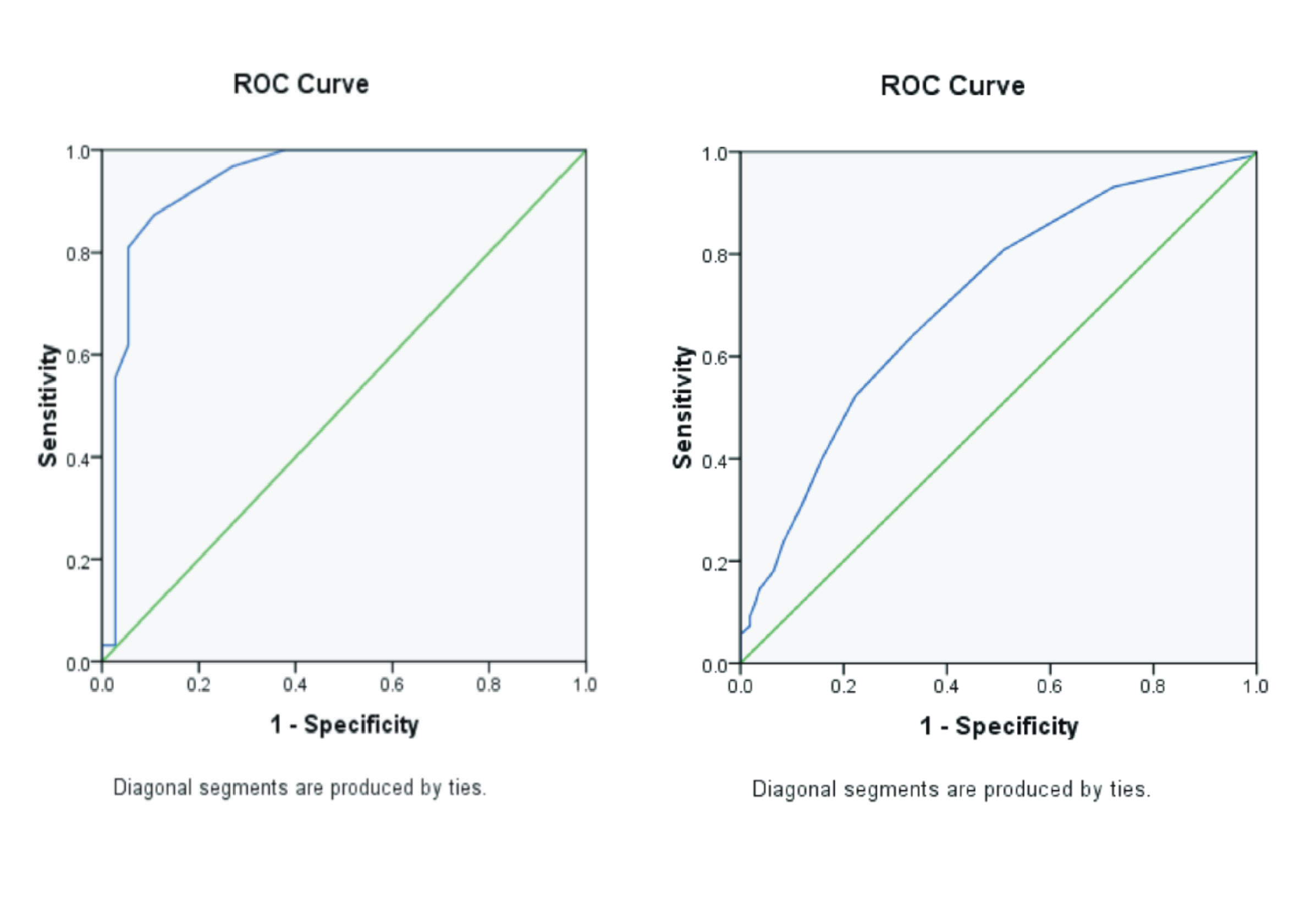
Background: HIV/AIDS cases continue to increase globally. A person with a weak immune system, especially people with HIV/AIDS, is very susceptible to various diseases, such as tuberculosis. Tuberculosis infection can be associated with HIV-positive individuals, which is caused by damage to cellular immunity due to the reduced number and function of CD4 cells. Purpose: To determine the profile of HIV/AIDS patients with TB coinfection based on CD4 values in RSUD Ibnu Sina Gresik. Method: The method used is observational analytical cross-sectional. Patients with TB and HIV coinfection were recapitulated from the Case Report Form (CRF). The results are presented in a frequency distribution table. Result: The study obtained information about 36 people with TB co-infected HIV/AIDS cases. Patients with CD4 values <200 cells/mm3 were 35 people (97.22%), and most of them were in the age group of 20-60 years were 35 people (97.22%). Male patients (83.33 %) dominate compared to female patients (16.67%). The duration of TB coinfection in HIV/AIDS patients occurs in less than one month, which is 21 people (58.33%). Conclusion: The profile of HIV/AIDS patients co-infected with TB is based on CD4 values that are more dominant in men, with the highest age being 20 - 60 years.
Abdallah, T.M., Ali, A.A.A., 2012. Epidemiology of tuberculosis in Eastern Sudan. Asia Pacific J. Trop. Biomidicine Vol.2(12), Pp 999-1001.
Carvalho, B.M. de, Monteiro, A.J., Neto, R. da J.P., Grangeiro, T., Frota, C.C., Barbosa, 2008. Factor Related to HIV/Tuberculosis Coinfection in a Brazilian Reference Hospital. Brazilian J. Infect. Dis. Vol. 12(4), Pp. 281-286.
Dafitri, I.A., Medison, I., Mizarti, D., 2020. Laporan Kasus TB Paru Koinfeksi HIV/AIDS. Departemen Pulmonologi dan Kedokteran Respirasi, Fakultas Kedokteran Universitas Andalas/RSUP DR. M. Djamil Padang, Indonesia. Yars. Med. J. Vol. 28(2), Pp. 021-031.
Eddy, S., S.Y., S., Reviono, H.M.Q.L., 2012. Profil Pasien Koinfeksi Tuberkulosis-HIV di RS Moewardi Surakarta 2010- 2011. J. Respirologi Indones. Vol 32(2), Pp. 85-88.
Fauziah, N., 2019. Prevalensi Tuberkulosis pada Pasien HIV Koinfeksi Tuberkulosis di RSU Haji Surabaya Periode 2016-2018. Universitas Airlangga.
Green, C.W., 2016. HIV dan TB. In: Zacky, A. (Ed.), HIV Dan AIDS. Yayasan Spiritia, Jakarta Pusat. Pp. 1-37.
Kemala, F., 2021. Tes CD4. Hello Sehat. URL https://hellosehat.com/seks/hivaids/cd4/ (accessed 11.19.21).
Kementrian Kesehatan RI, 2019. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MENKES/90/2019 Tentang Pedoman Nasional Pelayanan Kedokteran Tata Laksana HIV. HK.01.07/MENKES/90/2019.
Kementrian Kesehatan RI, 2020. Infodatin Situasi Penyakit HIV AIDS di Indonesia: Ditjen P2P (Sistem Informasi HIV/AIDS dan IMS (SIHA). Jakarta Selatan.
Khairani, K., 2020. Laporan Situasi Perkembangan HIV AIDS dan PIMS di Indonesia, Triwulan IV Tahun 2019. Jakarta.
Ladyani, F., Kristianingsih, A., 2019. Hubungan Antara Jumlah CD4 Pada Pasien yang Terinfeksi HIV/AIDS dengan Infeksi Oportunistik di Rumah Sakit Umum Abdul Moeloek Bandar Lampung Tahun 2016. JK Unila J. Kedokt. Univ. Lampung Vol. 3(1), Pp. 34-41.
Manurung, A., 2018. Faktor Risiko Kejadian Koinfeksi TB-HIV pada ODHA di Layanan Komite AIDS HKBP Tahun 2018. Universitas Sumatra Utara.
Mitku, A.A., Dessie, Z.G., Muluneh, E.K., Workie, D.L., 2016. Prevelance and Associated if TB-HIV Co-infection among HIV Infected Patients in Amhara Region, Ethiopia. African Heal. Sci. Vol. 16(2), Pp. 588-595.
Mulyadi, M., Fitrika, Y., 2010. Hubungan Tuberkulosis dengan HIV/AIDS. IDEA Nurs. J. Vol. 2(2), Pp. 162-166.
Muna, N., Cahyati, W.H., 2019. Determinan Kejadian Tuberkulosis pada Orang dengan HIV/AIDS. Higeia J. Public Heal. Reaserch Dev. Vol. 3(2), Pp. 168-178.
Nasarudin, J., N, A.U.Z., Karjadi, T.H., Rumende, M., 2016. Prevalensi Kejadian Resistensi Rifampisin pada Pasien TB-HIV dan Faktor-Faktor yang Mempengaruhi. CHEST Indones. J. Crit. Emerg. Med. Vol. 3(1), Pp. 11-17.
Nzou, C., Kambarami, R.A., Onyango, F.E., Ndhlovu, C.E., Chikwasha, V., 2010. Clinikal Predictors of Low CD4 Count among HIV Infected Pulmonary Tuberculosis Clients:A Health Facility-based Survey. South African Med. J. Vol. 100(9), Pp. 602-605.
Pramarta, D.Y., S, D.D., Gayatri, A.Y., Utama, M.S., Somia, A., M, T.P., 2019. Karakteristik pasien HIV/AIDS dengan Koinfeksi Tuberkulosis pada Poliklinik VCT RSUP Sanglah. Medicina (B. Aires). Vol. 50(2), Pp. 283-290.
Peraturan Menteri Kesehatan Republik Indonesia, 2015. Peraturan Menteri Kesehatan Republik Indonesia Nomor 87 Tahun 2014 tentang Pedoman Pengobatan Antiretroviral.
Permitasari, D.A., Sofro, S., Udji, M.A., 2012. Faktor Risiko Terjadinya Kinfeksi Tuberkulosis pada Pasien HIV/AIDS di RSUP DR Kariadi Semarang. Universitas Diponegoro.
Rangkuti, A.Y., Sarumpaet, S.M., Rasmaliah, 2013. Penderita AIDS dan Infeksi Opurtunistik di Rumah Sakit Umum Pusat (RSUP) H. Adam Malik Medan Tahun 2012. Gizi, Kesehat. Reproduksi dan Epidemiol. Vol. 2(5), Pp. 1-16.
Seitz, R., Paul-Ehrlich, 2016. Human Immunodeficiency Virus (HIV). Transfus Med. Hemotheraphy Vol. 43, Pp. 203-222.
Sharma, S., Dhungana, G.P., Pokhrel, B.M., Rijal, B.P., 2010. Opportunistic Infections in Relationto CD4 Level Among HIV Seropositive Patients from Central Nepal. Nepal Med Coll J. Vol. 12(1), Pp. 1-4.
Sukmaningrum, A., 2017. Memanfaatkan Usia Produktif dengan Usaha Kreatif Industri Pembuatan Kaos pada Remaja di Gresik. Paradigma Vol. 5(3), Pp. 1-6.
Taha, M., Deribew, A., Tessema, F., Assegid, S., Duchateau, L., Colebunders, R., 2011. Risk Factors of Active Tuberculosis in People Living with HIV/AIDS in Southwest Ethiopia: A Case Control Study. Ethiophian J. Heal. Sci. Vol. 21(2), Pp. 131-139.
World Health Organization (WHO), 2020. World Health Organization HIV update.
Yusuf, N.F., 2017. Karakteristik Penderita Hiv/Aids dengan Koinfeksi Tuberkulosis Paru di Rumah Sakit Umum Pusat Wahidin Sudirohusodo Makassar Periode Januari Sampai Juni 2016. Universitas Hasanuddin.
Copyright (c) 2022 Journal of Vocational Health Studies

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- The authors agree to transfer the transfer copyright of the article to the Journal of Vocational Health Studies (JVHS) effective if and when the paper is accepted for publication.
- Legal formal aspect of journal publication accessibility refers to Creative Commons Attribution-NonCommercial-ShareAlike (CC BY-NC-SA), implies that publication can be used for non-commercial purposes in its original form.
- Every publications (printed/electronic) are open access for educational purposes, research, and library. Other that the aims mentioned above, editorial board is not responsible for copyright violation.
Journal of Vocational Health Studies is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License