BACTERIAL PROFILE AND ANTIBIOTIC SUSCEPTIBILITY TEST AMONG DIABETES MELLITUS PATIENTS WITH GANGRENE IN SURABAYA

Downloads
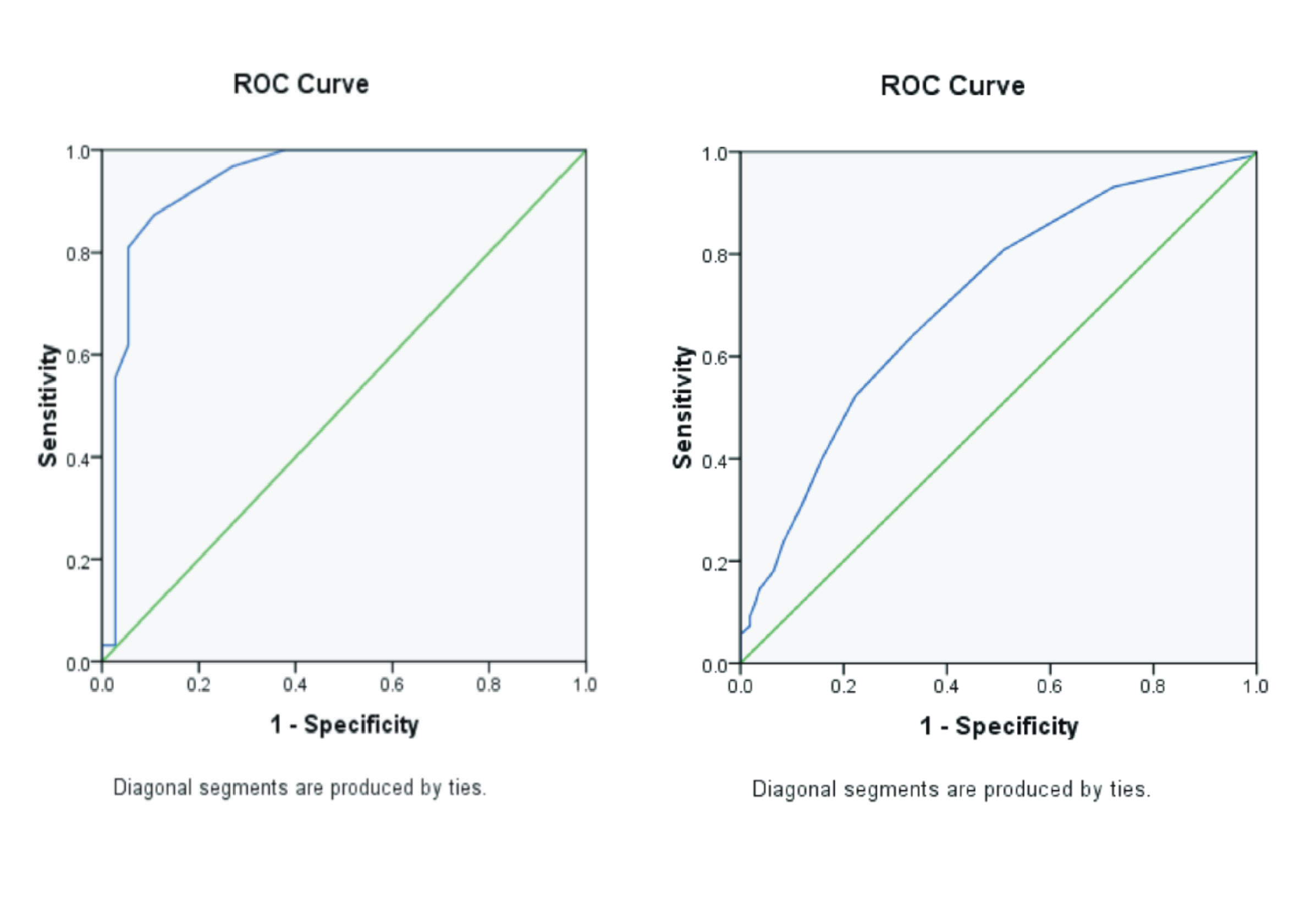
Background: Gangrene is a severe complication of damaged tissue that can occur in people with Diabetes Mellitus (DM), putting them at risk for bacterial infection. A pus culture can show diabetic gangrene patients' infecting bacteria. Purpose: Determine the prevalence of infection-causing bacteria and antibiotic sensitivity tests in diabetic gangrene patients at Haji Regional General Hospital, East Java Province, for January-December 2021. Method: The method used in this study is observational analytical cross-sectional, which is based on secondary data and is analyzed using the percentage formula and Chi-Square test. Result: The data obtained from 39 patients revealed 29 (74.4%) positive patients for bacterial infection. The Gram-negative bacteria was found to cause infection more frequently (72.41%) than the Gram-positive bacteria (27.59%). The prevalence of Gram-negative bacteria species most frequently from Escherichia coli (ESBL) 13.79% (4/29), Klebsiella pneumoniae 10.35% (3/29), Proteus mirabilis 10.35% (3/29). While the dominant Gram-positive bacteria a Methicillin-Resistant Staphylococcus aureus (MRSA) 10.35% (3/29). The antibiotic sensitivity test showed that Gram-negative group were susceptible to ertapenem, meropenem, amikacin, gentamicin, and piperacillin tazobactam while resistant to ampicillin and cefazolin. The antibiotic sensitivity tests showed that the Gram-positive group was susceptible to linezolid, vancomycin, and tigecycline while resistant to tetracycline and ciprofloxacin. Conclusion: It is important to screen the bacterial profile causing gangrene and their antibiotic susceptibility pattern in DM patients in order to give proper treatment to DM patients.
Agbi, K.E., Carvalho, M., Phan, H., Tuma, C., 2017. Case Report: Diabetic Foot Ulcer Infection Treated with Topical Compounded Medications. Intern. J. Pharm. Compd. Vol. 21(1), Pp. 22-27.
Akhi, M.T., Ghotaslou, R., Asgharzadeh, M., Varshochi, M., Pirzadeh, T., Memar, M.Y., Bialvaei, A.Z., Sofla, H.S.Y., Alizadeh, N., 2015. Bacterial Etiology and Antibiotic Susceptibility Pattern of Diabetic Foot Infections in Tabriz, Iran. GMS Hyg. Infect. Control Vol. 10(2).
Al-Rubeaan, K., Derwish, M. Al, Ouizi, S., Youssef, A.M., Subhani, S.N., Ibrahim, H.M., Alamri, B.N., 2015. Diabetic Foot Complications and Their Risk Factors from A Large Retrospective Cohort Study. PLoS One Vol.10(5), Pp. e0124446.
Alhubail, A., Sewify, M., Messenger, G., Masoetsa, R., Hussain, I., Nair, S., Tiss, A., 2020. Microbiological Profile of Diabetic Foot Ulcers in Kuwait. PLoS One Vol. 15(12), Pp. e0244306.
AlSadrah, S.A., 2019. Impaired Quality of Life and Diabetic Foot Disease in Saudi Patients with Type 2 Diabetes: A Cross-Sectional Analysis. SAGE Open Med. Vol.7, Pp. 2050312119832092.
Apelqvist, J., Elgzyr, T., Larsson, J., Londahl, M., Nyberg, P., Thorne, J., 2011. Factors Related to Outcome of Neuroischemic/Ischemic Foot Ulcer in Diabetic Patients. J. Vasc. Surg. Vol. 53(6), Pp.1582-8.e2.
Belefquih, B., Frikh, M., Benlahlou, Y., Maleh, A., Jadid, L., Bssaibis, F., Ghazouani, M., Chagar, B., Lamsaouri, J., Lemnouer, A., Elouennass, M., 2016. Diabetic Foot Infection in Morocco: Microbiological Profile. Wounds Vol. 28(3), Pp. 89-98.
Chen, Y., Ding, H., Wu, H., Chen, H.-L., 2017. The Relationship Between Osteomyelitis Complication and Drug-Resistant Infection Risk in Diabetic Foot Ulcer: A Meta-analysis. Int. J. Low. Extrem. Wounds Vol. 16(3), Pp. 183-190.
Du, F., Ma, J., Gong, H., Bista, R., Zha, P., Ren, Y., Gao, Y., Chen, D., Ran, X., Wang, C., 2022. Microbial Infection and Antibiotic Susceptibility of Diabetic Foot Ulcer in China: Literature Review. Front Endocrinol Vol.19(13), Pp. 881659.
Dubsky, M., Jirkovska, A., Bem, R., Skibova, V.F.J., Schaper, N.C., Lipsky, B.A., 2013. Risk Factors for Recurrence of Diabetic Foot Ulcers: Prospective Follow-Up Analysis in The Eurodiale Subgroup. Intern. Wound J. Vol. 10(5), Pp. 555-561.
Gershater, M.A., Londahl, M., Nyberg, P., Larsson, J., Thorne, J., Eneroth, M., Apelqvist, J., 2009. Complexity of Factors Related to Outcome of Neuropathic and Neuroischaemic/Ischaemic Diabetic Foot Ulcers: A Cohort Study. Diabetologia Vol. 52(3), Pp. 398-407.
Heravi, F.S., Zakrzewski, M., Vickery, K., Armstrong, D.G., Hu, H., 2019. Bacterial Diversity of Diabetic Foot Ulcers: Current Status and Future Prospectives. J. Clin. Med. Vol. 8(11), Pp. 1935.
International Diabetes Federation (IDF), 2019. IDF Diabetes Atlas, 9 th. ed. International Diabetes Federation (IDF).
Johannesson, A., Larsson, G.-U., Ramstrand, N., Turkiewicz, A., Wirrhn, A.-B., Atroshi, I., 2009. Incidence of Lower-Limb Amputation in The Diabetic and Nondiabetic General Population: A 10-year Population-Based Cohort Study of Initial Unilateral and Contralateral Amputations and Contralateral Amputations and Reamputations Reamputations. Diabetes Care Vol. 32(2), Pp. 275-280.
Kaur, M., Dhillon, M., Angrup, A., Rangasamy, K., 2022. Polymicrobial Infection Presenting as Non-Clostridial Gas Gangrene in A Non-Diabetic Trauma Patient. Interantional J. Burn. Trauma Vol. 12(5), Pp. 194–203.
Olid, A.S., Ivan Sola, L.A.B.-N., Gianneo, O.D., Cosp, X.B., Lipsky, B.A., 2015. Systemic Antibiotics for Treating Diabetic Foot Infections. Cochrane Database Syst. Rev. Vol. 4(9), Pp. CD009061.
Saltoglu, N., Ergonul, O., Tulek, N., Yemisen, M., Kadanali, A., Karagoz, G., Batirel, A., Ak, O., Sonmezer, C., Eraksoy, H., Cagatay, A., Surme, S., Nemli, S.A., Demirdal, T., Coskun, O., Ozturk, D., Ceran, N., Pehlivanoglu, F., Sengoz, G., Aslan, T., Akkoyunlu, Y., Oncul, O., Ay, H., Mulazımoglu, L., Erturk, B., Yilmaz, F., Yoruk, G., Uzun, N., Simsek, F., Yildirmak, T., Yaşar, K.K., Sonmezoglu, M., Kucukardali, Y., Tuna, N., Karabay, O., Ozgunes, N., Sargın, F., 2018. Influence of Multidrug Resistant Organisms on The Outcome of Diabetic Foot Infection. Int. J. Infect. Dis. Vol. 70, Pp. 10-14.
Schaper, N.C., Netten, J.J. Van, Apelqvist, J., Lipsky, B.A., Bakker, K., Foot, I.W.G. on the D., 2016. Prevention and Management of Foot Problems in Diabetes: A Summary Guidance for Daily Practice 2015, Based on The IWGDF Guidance Documents. Diabetes. Metab. Res. Rev. Vol 32(Suppl. 1), Pp. 7-15.
Spreen, M.I., Gremmels, H., Teraa, M., Sprengers, R.W., Verhaar, M.C., Eps, R.G.S. van, Vries, J.-P.P.M. de, Mali, W.P.T.M., Overhagen, H. van, PADI, Groups, J.S., 2016. Diabetes is Associated with Decreased Limb Survival in Patients with Critical Limb Ischemia: Pooled Data from Two Randomized Controlled Trials. Diabetes Care Vol. 39(11), Pp. 2058-2064.
Tang, Z.Y., 2019. The Comprehension to The Part of Diabetic Foot Infection. In: Chinese Guideline on Prevention and Management of Diabetic Foot. World Clini Drugs. Vol. 40(9). Pp. 599-602.
Tong, T., Yang, C., Tian, W., Liu, Z., Liu, B., Cheng, J., Cheng, Q., Zhou, B., 2020. Phenotypes and Outcomes in Middle-Aged Patients with Diabetic Foot Ulcers: A Retrospective Cohort Study. J. Foot Ankle Res. Vol. 24.
Uckay, I., Lubbeke, A., Harbarth, S., Emonet, S., Tovmirzaeva, L., Agostinho, A., Longtin, Y., Peter, R., Hoffmeyer, P., Pittet, D., 2012. Low Risk Despite High Endemicity of Methicillin-Resistant Staphylococcus aureus Infections Following Elective Total Joint Arthroplasty: A 12-Year Experience. Ann. Med. Vol. 44(4), Pp. 360-368.
Varaiya, A.Y., Dogra, J.D., Kulkarni, M.H., Bhalekar, P.N., 2008. Extended-Spectrum Beta-Lactamase-Producing Escherichia coli and Klebsiella pneumoniae in Diabetic Foot Infections. Indian J. Pathol. Microbioliolgy Vol. 51(3), Pp. 370-372.
Williams, D.T., Hilton, J.R., Harding, K.G., 2004. Diagnosing foot infection in diabetes. Clin. Infect. Dis. An Off. Publ. Infect. Dis. Soc. Am. United States Vol. 1(Suppl. 39), Pp. S83-6.
Yan, X., Song, J., Zhang, L., Li, X., 2022. Analysis of Risk Factors for Multidrug-Resistant Organisms in Diabetic Foot Infection. BMC Endocr. Disord. Vol. 46.
Copyright (c) 2024 Journal of Vocational Health Studies

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- The authors agree to transfer the transfer copyright of the article to the Journal of Vocational Health Studies (JVHS) effective if and when the paper is accepted for publication.
- Legal formal aspect of journal publication accessibility refers to Creative Commons Attribution-NonCommercial-ShareAlike (CC BY-NC-SA), implies that publication can be used for non-commercial purposes in its original form.
- Every publications (printed/electronic) are open access for educational purposes, research, and library. Other that the aims mentioned above, editorial board is not responsible for copyright violation.
Journal of Vocational Health Studies is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License