Maternal Nutrition: The Foundation of Breastfeeding and Beyond
Gizi Ibu: Fondasi Menyusui dan Masa Depan Anak

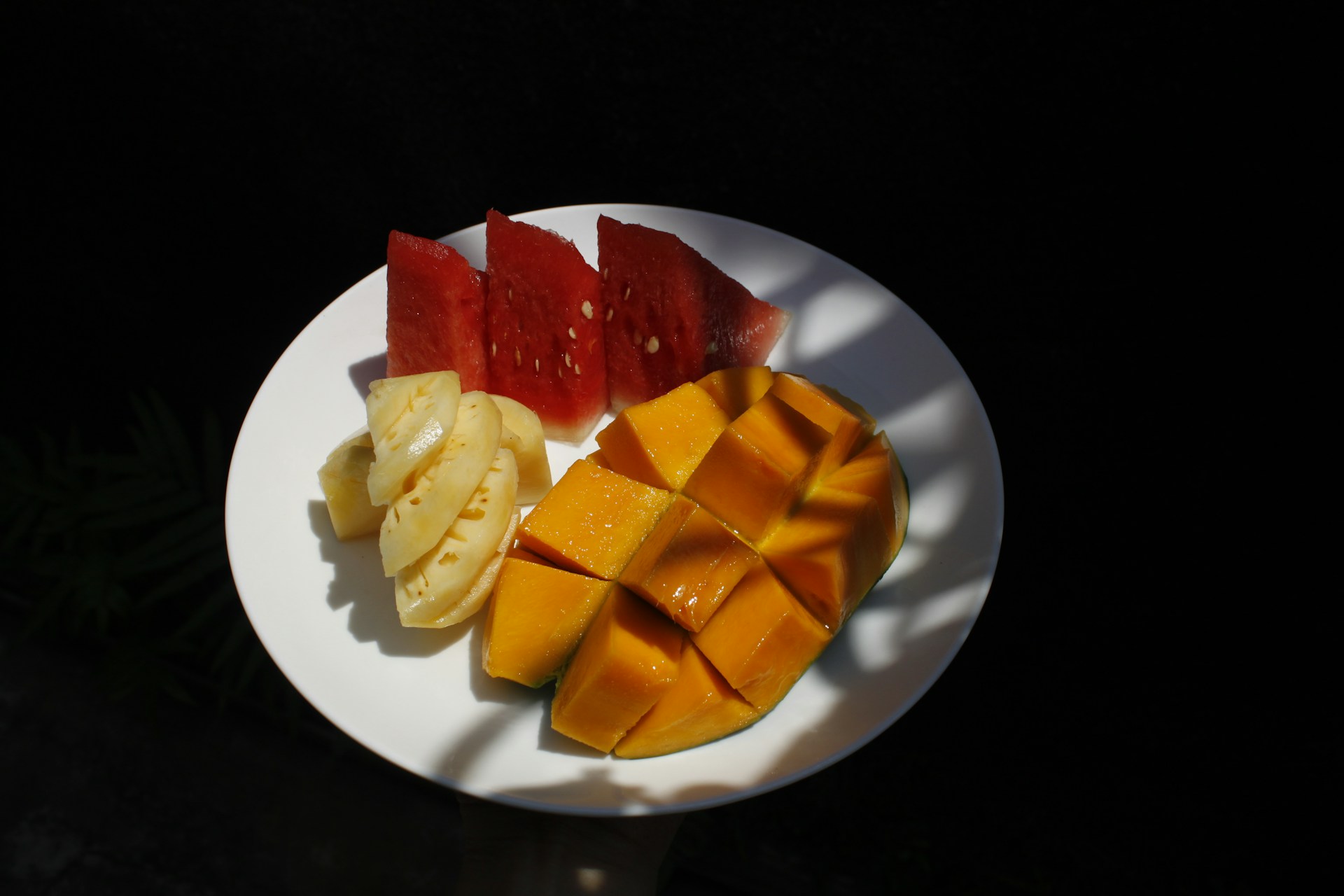
Background: Breastmilk from a healthy and well-nourished mother serves as the optimal source of nutrition for infant growth and development. The composition of breastmilk is affected by maternal dietary patterns. Beyond its nutritional value, breastfeeding fosters emotional bonding between the mother and infant.
Objectives: This study aims to explore the role of maternal nutrition in breastfeeding success and infant’s well-being through scientific and philosophical lenses.
Methods: Literature search was conducted via PubMed (Medline Database), including systematic reviews, meta-analyses, and original research articles published within the last decade (2014-2024). The following keywords were utilised: ("maternal nutrition" OR "maternal health" OR "breastfeeding practice" OR "breastmilk") AND ("neurodevelopment" OR "intellectual development" OR "child development"). Inclusion criteria comprised open-access articles, while studies were available only in abstract form were excluded.
Discussions: Breastmilk production requires an adequate intake of macronutrients, including protein, carbohydrates, and fats; thus, maternal dietary intake significantly affects breastmilk composition. The nutritional and bioactive components in breastmilk support the infant’s immune function, neurodevelopment, and physical growth, while simultaneously providing necessary energy for the lactating mother. Breastfeeding should be understood as a holistic practice that extends beyond nutrient transfer, necessitating multisectoral collaboration involving government, non-governmental organizations, healthcare providers, and the population at large.
Conclusions: Maternal well-being is intrinsically linked to child health, as well-nourished mothers provide a vital foundation for optimal infant development. A compassionate, community-based approach to maternal nutrition is an essential view that respects individual choices while emphasizing the importance of collective support to enhance the health and well-being of both mother and child.
WHO & UNICEF. Global strategy for infant and young child feeding. (WHO, Geneva, Switzerland & UNICEF, New York, NY, USA, 2003).
Bravi, F. et al. Dietary patterns of breastfeeding mothers and human milk composition: Data from the Italian medidiet study. Nutrients 13, 1722 (2021). https://doi.org/10.3390/nu13051722
Pham, Q., Patel, P., Baban, B., Yu, J. & Bhatia, J. Factors affecting the composition of expressed fresh human milk. Breastfeeding Medicine 15, 551-558 (2020). https://doi.org/10.1089/bfm.2020.0195
Keikha, M., Bahreynian, M., Saleki, M. & Kelishadi, R. Macro- and micronutrients of human milk composition: Are they related to maternal diet? A comprehensive systematic review. Breastfeeding Medicine 12, 517-527 (2017). https://doi.org/10.1089/bfm.2017.0048
Lucas, R., Amoo, T. B. & Popoola, T. Maternal nutrition and human milk nutrients: A scoping review. Journal of Human Lactation 40, 45-58 (2024). https://doi.org/10.1177/08903344211058498
Centers for Disease Control and Prevention. Maternal diet and breastfeeding. In: Breastfeeding special circumstances [Internet]. https://www.cdc.gov/breastfeeding-special-circumstances/hcp/diet-micronutrients/maternal-diet.html
Amoo, T. B., Popoola, T. & Lucas, R. Promoting the practice of exclusive breastfeeding: A philosophic scoping review. International Breastfeeding Journal 17, 32 (2022). https://doi.org/10.1186/s13006-022-00445-5
Modak, A., Ronghe, V. & Gomase, K. P. The psychological benefits of breastfeeding: Fostering maternal well-being and child development. Cureus (2023). https://doi.org/10.7759/cureus.46730
Else-Quest, N. M., Hyde, J. S. & Clark, R. Breastfeeding, bonding, and the mother-infant relationship. Merrill-Palmer Quarterly 49, 495-517 (2003). https://doi.org/10.1353/mpq.2003.0020
Marshall, N. E. et al. The importance of nutrition in pregnancy and lactation: Lifelong consequences. American Journal of Obstetrics and Gynecology 226, 607-632 (2022). https://doi.org/10.1016/j.ajog.2021.12.035
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Harrison, M. (ed.) Nutrition during pregnancy and lactation: Exploring new evidence: Proceedings of a workshop in brief. (National Academies Press, Washington DC, 2020). https://doi.org/10.17226/25831
Nommsen, L. A., Lovelady, C. A., Heinig, M. J. et al. Determinants of energy, protein, lipid and lactose concentrations in human milk during the first 12 mo of lactation: The DARLING Study. American Journal of Clinical Nutrition 53, 457-465 (1991).
Boix-Amorós, A. et al. Reviewing the evidence on breast milk composition and immunological outcomes. Nutrition Reviews 77, 541-556 (2019). https://doi.org/10.1093/nutrit/nuz019
Kleinman, R. E. & Greer, F. R. Pediatric nutrition, 7th ed. (American Academy of Pediatrics, Elk Grove Village, IL, 2013).
Andreas, N. J., Kampmann, B. & Mehring Le-Doare, K. Human breast milk: A review on its composition and bioactivity. Early Human Development 91, 629-635 (2015). https://doi.org/10.1016/j.earlhumdev.2015.08.013
Ares Segura, S., Arena Ansótegui, J. & Díaz-Gómez, M. The importance of maternal nutrition during breastfeeding: Do breastfeeding mothers need nutritional supplements? Anales de Pediatría (English Edition) 84(2016). https://doi.org/10.1016/j.anpede.2015.07.035
Cortés-Albornoz, M. C. et al. Maternal nutrition and neurodevelopment: A scoping review. Nutrients 13, 3530 (2021). https://doi.org/10.3390/nu13103530
Szyller, H. et al. Bioactive components of human milk and their impact on child’s health and development: Literature review. Nutrients 16, 1487 (2024). https://doi.org/10.3390/nu16101487
Innis, S. M. Impact of maternal diet on human milk composition and neurological development of infants. American Journal of Clinical Nutrition 99, 734S-741S (2014). https://doi.org/10.3945/ajcn.113.072595
Martins, B. P., Bandarra, N. M. & Figueiredo-Braga, M. The role of marine omega-3 in human neurodevelopment, including autism spectrum disorders and attention-deficit/hyperactivity disorder: A review. Critical Reviews in Food Science and Nutrition 60, 1431-1446 (2020). https://doi.org/10.1080/10408398.2019.1573800
Li, M. et al. Preconception and prenatal nutrition and neurodevelopmental disorders: A systematic review and meta-analysis. Nutrients 11, 1628 (2019). https://doi.org/10.3390/nu11071628
DeCapo, M., Thompson, J. R., Dunn, G. & Sullivan, E. L. Perinatal nutrition and programmed risk for neuropsychiatric disorders: A focus on animal models. Biological Psychiatry 85, 122-134 (2019). https://doi.org/10.1016/j.biopsych.2018.08.006
Adhikari, S. et al. Maternal dietary intake, nutritional status and macronutrient composition of human breast milk: Systematic review. British Journal of Nutrition 127, 1796-1820 (2021). https://doi.org/10.1017/S0007114521002786
Centers for Disease Control and Prevention. Maternal diet and breastfeeding. In: Breastfeeding special circumstances[Internet]. (2024) [cited 2025 Mar 2]. Available from: https://www.cdc.gov/breastfeeding-special-circumstances/hcp/diet-micronutrients/maternal-diet.html
Picciano, M. F. Nutrient requirements during pregnancy and lactation. Nutrients 13, 692 (2021). https://doi.org/10.3390/nu13020692
Moran, V. H. et al. Nutrition for optimal lactation. Annals of Nutrition and Metabolism 79, 257-266 (2023). https://doi.org/10.1159/000541757
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Harrison M, editor. Nutrition during pregnancy and lactation: Exploring new evidence: Proceedings of a workshop. Washington (DC): National Academies Press (US); 2020 Jul 31. Chapter 7, Maternal intakes and nutritional status during lactation and the implications for maternal and infant health. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562621/
Cimmino F, Catapano A, Petrella L, Villano I, Tudisco R, Cavaliere G. Role of milk micronutrients in human health. Front. Biosci. (Landmark Ed) 28, 41 (2023). https://doi.org/10.31083/j.fbl2802041
Houweling T.A., Grünberger I. Intergenerational transmission of health inequalities: Towards a life course approach to socioeconomic inequalities in health-a review. Journal of Epidemiology and Community Health 78, 641-649 (2024). https://doi.org/10.1136/jech-2022-220162
Van Abeelen A.F., Veenendaal M.V., Painter R.C., de Rooij S.R., Dijkgraaf M.G., Bossuyt P.M. et al. Survival effects of prenatal famine exposure. The American Journal of Clinical Nutrition 95, 179-183 (2012). https://doi.org/10.3945/ajcn.111.022038
Schulz L.C. The Dutch Hunger Winter and the developmental origins of health and disease. Proceedings of the National Academy of Sciences 107, 16757-16758 (2010). https://doi.org/10.1073/pnas.1012911107
Lokossou Y.U., Tambe A.B., Azandjèmè C., Mbhenyane X. Socio-cultural beliefs influence feeding practices of mothers and their children in Grand Popo, Benin. Journal of Health, Population and Nutrition 40, 1 (2021). https://doi.org/10.1186/s41043-021-00258-7
Tomori C. Global lessons for strengthening breastfeeding as a key pillar of food security. Frontiers in Public Health11, 1256390 (2023). https://doi.org/10.3389/fpubh.2023.1256390
Afandi M., Anomsari E., Novira A., Sudartini S. A penta-helix approach to collaborative governance of stunting intervention in West Java Indonesia. In: Proceedings of the Third International Conference Administration Science, ICAS 2021, Bandung, Indonesia, 15 Sept 2021 (2022). https://doi.org/10.4108/eai.15-9-2021.2315238
Sjögren Forss K., Kottorp A., Rämgård M. Collaborating in a penta-helix structure within a community based participatory research programme: ‘Wrestling with hierarchies and getting caught in isolated downpipes’. Archives of Public Health 79, 1 (2021). https://doi.org/10.1186/s13690-021-00544-0
Srivastava K., Norman A., Ferrario H., Mason E., Mortimer S. A qualitative exploration of the media's influence on UK women's views of breastfeeding. British Journal of Midwifery 30, 1 (2022).
World Health Organization. Approaches to community-based breastfeeding promotion and support. In: Community-based strategies for breastfeeding promotion and support in developing countries. Geneva: WHO; 2003.
Bardosono S., Hildayani R., Chandra D.N., Basrowi R.W., Wibowo Y. The knowledge retention after continuing health education among midwives in Indonesia. Medical Journal of Indonesia 27, 128-133 (2018).
World Health Organization. INSPIRE handbook: Action for implementing the seven strategies for ending violence against children. Geneva: WHO; 2018.
Mahumud R.A., Uprety S., Wali N., Renzaho A.M., Chitekwe S. The effectiveness of interventions on nutrition social behaviour change communication in improving child nutritional status within the first 1000 days: Evidence from a systematic review and meta‐analysis. Maternal & Child Nutrition 18, e13286 (2021). https://doi.org/10.1111/mcn.13286
Dinour L.M., Rivera Rodas E.I., Amutah-Onukagha N.N. et al. The role of prenatal food insecurity on breastfeeding behaviors: Findings from the United States pregnancy risk assessment monitoring system. International Breastfeeding Journal 15, 30 (2020). https://doi.org/10.1186/s13006-020-00276-x
de Brito J.N., Friedman J.K., Johnson S.T., Berge J.M., Mason S.M. Exploring the associations of food and financial insecurity and food assistance with breastfeeding practices among first-time mothers. Public Health Nutrition 27, 1 (2024). https://doi.org/10.1017/s1368980024001514
World Health Organization. Guideline: Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. Geneva: WHO; 2017.
Pérez‐Escamilla R., Martinez J.L., Segura‐Pérez S. Impact of the baby‐friendly hospital initiative on breastfeeding and child health outcomes: A systematic review. Maternal & Child Nutrition 12, 402-417 (2016). https://doi.org/10.1111/mcn.12294
Basrowi R.W., Sulistomo A.W., Adi N.P., Widyahening I.S., Vandenplas Y. Breastfeeding knowledge, attitude, and practice among white-collar and blue-collar workers in Indonesia. Journal of Korean Medical Science 34, 45 (2019).
Basrowi R.W., Sulistomo A.B., Adi N.P., Vandenplas Y. Benefits of a dedicated breastfeeding facility and support program for exclusive breastfeeding among workers in Indonesia. Pediatric Gastroenterology, Hepatology & Nutrition 18, 94-99 (2015).
Basrowi R.W., Khoe L.C., Yosia M. Prevalence of breastfeeding and its supporting factors during COVID-19 pandemic in Indonesia. General Medicine 25, 5 (2023).
Basrowi R.W., Sastroasmoro S., Sulistomo A.W., Bardosono S., Hendarto A., Soemarko D.S. et al. Developing a workplace lactation promotion model in Indonesia using Delphi technique. Archives of Public Health 76, 1-9 (2018).
Basrowi R.W., Darus F., Partiwi I.G.A.N., Sutanto L.B., Sulistomo A., Soemarko D.S. et al. The strategic effort to ensure successful breastfeeding practice in the workplace: An Indonesian expert opinion. The Open Public Health Journal 17, 1 (2024).
Copyright (c) 2025 Amerta Nutrition

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
AMERTA NUTR by Unair is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
1. The journal allows the author to hold the copyright of the article without restrictions.
2. The journal allows the author(s) to retain publishing rights without restrictions
3. The legal formal aspect of journal publication accessibility refers to Creative Commons Attribution Share-Alike (CC BY-SA).
4. The Creative Commons Attribution Share-Alike (CC BY-SA) license allows re-distribution and re-use of a licensed work on the conditions that the creator is appropriately credited and that any derivative work is made available under "the same, similar or a compatible license”. Other than the conditions mentioned above, the editorial board is not responsible for copyright violation.